
Correlating quadriceps patellar tendon angle and lateral patellar tilt angle in patients with irregular alignment: a cross-sectional study with retrospective data
Introduction
The knee joint is a complex articulation that allows interaction between bony and soft tissue structures to maintain balance (1). The morphology of the knee joint has been extensively examined over the past few decades and individual anatomical malalignment have been reported. While most studies have addressed features of a single bone, specifically the femur, only a few studies have described the entire knee joint (2). Detailed morphological descriptions covering the entire joint are rare and little is known about the relationship of anatomical measurements to each other and gender, chondromalacia, fad pad edema (3).
Patellar tendon length, patellar height, tibial tubercle-trochlear groove distance (TT-TG), patella angle (PA), trochlear sulcus angle (TSA), trochlear groove depth (TGD), medial trochlea length (MT), lateral trochlea length (LT), medial trochlear/lateral trochlear length ratio (MT/LT), lateral patellar tilt angle (LPTA), patella-patellar tendon angle (PPTA), quadriceps patellar tendon angle (QPA), Insall-Salvati index (ISI), medial trochlear inclination (MTI), lateral trochlear inclination (LTI) are measurements providing us information about the development of anterior knee pain, trochlear dysplasia, patellofemoral instability, and patellofemoral malalignment. These malalignment may be associated with peripatellar fat pad edema, chondromalacia, and one of the underlying conditions which may cause patients more prone to ligament injury (4). The decrease in LPTA may lead to increased pressure on the lateral aspect of the knee and cause patellar or femoral cartilage damage (5). Especially PPTA, QPA, LPTA, and trochlear depth values were significantly lower in patients with patellofemoral malalignment and in women in the recent literature data (6). LPTA has high sensitivity and specificity in showing the patellofemoral malalignment and instability and is also associated with increased TT-TG distance, patella Alta, trochlear dysplasia, and medial patellofemoral ligament pathologies (4,7,8).
QPA is newly described angle. QPA represents the angular sum of the total forces transmitted to the patella by the quadriceps and the patellar tendon. As the QPA increases, the vectorial force applied to the patella also increases. Although QPA is an angle used in the diagnosis of patellofemoral instability and pain syndrome (4,9).
In our study, we plan to reveal the importance of anatomical malalignment related to the knee joint by measuring the patellar tendon length, patellar height, LPTA, PPTA, QPA, MTI and LTI, PA, TSA, TGD, MT, LT, MT/LT ratio, TT-TG distance, ISI. Thus, we aim to contribute to a better understanding of patellofemoral malalignment. We aim to reveal the relationship of these anatomical malalignment with pathologies such as fat-pad edema, patellar chondromalacia, effusion, and gender factor. In addition, we aim to reveal whether there is a significant relationship between two important angles LPTA and QPA and whether there is a significant increase in the development of chondromalacia for the patient group with LPTA >5°. The clinical relevance of the findings in current study may underline the complex relationship between LPTA, QPA and various anatomical parameters in the knee joint. We present this article in accordance with the STROBE reporting checklist (available at https://qims.amegroups.com/article/view/10.21037/qims-23-1592/rc).
Methods
The patient cohort
A cross-sectional study with retrospective data was conducted. Three hundred and fifty patients who underwent knee magnetic resonance imaging (MRI) examinations between January 2018 and March 2020 were examined. A total of 73 patients who have previous knee surgery, prosthesis, cystic or solid lesions involving the knee joint and popliteal fossa, severe osteoarthritis and meniscal disease, Osgood-Schlatter disease, patellar subluxation, previous chemoradiotherapy, and known systemic disease were excluded from our study. Because many of our measurements were also affected by knee position, many patients who underwent MRI before inappropriate positioning had to be excluded from our study. During MRI examination, a standard flexion posture of 10–15 degrees was provided by the coil. A total of 277 knee MRI patients, 158 women, and 119 men, were included in our study. The included patients were divided into those with an LPTA of ≤5° and those with >5° LPTA.
LPTA >5° is accepted as a abnormal patient group and cases with LPTA ≤5° are accepted as the control group (4). Of 33 participants’ LPTA were ≤5°, and 244 patients had LPTA >5°.
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Ethics committee approval was obtained from a Local Scientific Research Ethics Committee (decision number: 137, date: June 30, 2021). And individual consent for this retrospective analysis was waived. MRI of all subsequent was assessed by a radiologist with 7-year experience in the field of musculoskeletal imaging.
The study design
The patellar tendon length, patellar height, LPTA, PPTA, QPA, MTI and LTI, PA, TSA, TGD, MT, LT, MT/LT, TT-TG distance, ISI were measured for each patient. The mean values, standard deviations, and whether the measurement or angle differs significantly by gender were investigated for each measurement, respectively. Mean LPTA was calculated for both the patient group (LPTA >5°) and the control group (LPTA ≤5°). It was investigated whether there was a relationship between the two groups in terms of the development and grade of chondromalacia. It was evaluated whether chondromalacia severity (grade) increased as LPTA increased.
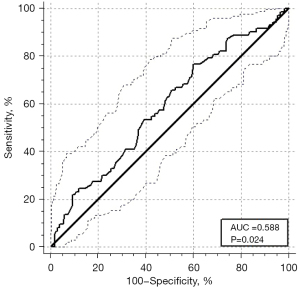
Mean QPA was calculated for two groups (LPTA >5° and ≤5°), and it was examined whether QPA increased as LPTA increased. It was investigated whether there was a significant difference between the patient group and the control group in terms of the patellar tendon length, patellar height, PPTA, QPA, MTI, LTI, PA, TSA, TGD, MT, LT, MT/LT, TT-TG distance, ISI, the presence of pathologies such as fat-pad edema, effusion, and chondromalacia Whether the patellar tendon length, LPTA, PPTA, QPA, MTI and LTI, PA, TSA, TGD, MT, LT, MT/LT ratio, TT-TG distance, ISI measurements changed significantly as QPA increased is investigated. In addition, it was evaluated whether the frequency of fat-pad edema, effusion, and chondromalacia increased as QPA increased. The cut-off value was determined for LPTA causing fat pad edema is calculated. Cut-off values were calculated for patellar tendon length and patellar height in order to predict with higher sensitivity the presence of patella Alta where ISI is >1.3. Receiver operating characteristic (ROC) curve was drawn for these cutoff values (4).
Measurements
LPTA was assessed on axial MRI fat-suppressed proton density (PD) images by measuring the angle between the transverse axis of the patella and the line drawn parallel to the line connecting the most posterior parts of femoral condyles. While measuring on the transverse axis, the axial image in which the largest diameter of the patella is observed was chosen. And for the second line, an axial image is selected where the femoral condyles are at the most posterior and the line forming the transverse axis of the patella.
PPTA, QPA, and ISI were measured in the midsagittal plane, where the quadriceps tendon, patellar tendon, and the upper and lower ends of the patella were can be seen. PPTA is measured as the crossing angle between a line connecting the upper and lower ends of the patella and a line from the inferior patella to the tibial tuberosity. QPA is measured as the angle between the intersection of two lines, which is representing the long axis of the patellar and quadriceps tendons (4). ISI is obtained as the ratio of the patellar tendon length to the patellar height. Patellar tendon length is measured by drawing a line of the posterior surface of the tendon from the lower end of the patella to the point of attachment to the tibia. Patellar length is obtained as the greatest pole-to-pole distance on midsagittal images.
On axial PD images, MTI is measured as the angle between the lateral trochlear facet and the transcondylar axis. LTI is measured as the angle between the lateral trochlear facet and the transcondylar axis. The distance between the base of the trochlear and the vertical line connecting the most anterior points of the medial and lateral facets is measured as TGD, on axial images. PA is obtained as the angle between the medial and lateral facets of the patella. TT-TG is measured as a distance from the apex of the tibial tuberosity to the base of the trochlear groove. TSA is measured as the angle between the medial and lateral trochlear facets (Figure 1). For LPTA, LTI, MTI, and TSA angles, there was always a single slice that would meet certain conditions, and the operator made 3 measurements on that slice and noted the average value in Excel. In LPTA, LTI, MTI, and TSA, the axial image showing the patellar axis at the widest was preferred. For LTI and MTI, we had only one cross-section to choose from. It was the first cranial axial slice showing the trochlear cartilage at most. In order to have a standard in our measurements, TSA was also performed on the slice preferred for LTI measurement.When measuring MT/LT, multiple measurements were performed on more than one slice. The 3 cm cranial slice of the tibiofemoral joint was selected. Since this selection was performed approximately, the measurement was repeated at least 2 times. Simultaneously, TGD was measured on these slices. While measuring patellar height and patellar tendon length, the measurement was performed more than once on more than one slice, as the anterior cruciate ligament is best visible and there are generally 2–3 slices that correspond to the midline of the patella in the sagittal plane. While QPA and ISI measurements were also made, more than one measurement was made in more than one slice. And the average measurement value was noted.

Chondromalacia is classified as four grades by MRI on PD images. Grade 1 and 2 are accepted as low grade. Grade 3 and 4 are classified as high grade (4-6) (Figure 2). Grade 1: cartilage signal abnormality is observed, yet the architectural integrity remains intact. Grade 2: focal defects are noted, encompassing less than 50% of the cartilage thickness. Grade 3: cartilage loss more than 50% of the cartilage thickness, without concurrent bone edema. Grade 4: full-thickness cartilage defect or loss is observed, accompanied by associated bone marrow edema (4-6). Fat-pad oedema classified into groups, according to its location (Superolateral Hoffa, Non Superolateral Hoffa, Prefemoral, Suprapatellar).

MRI protocol and image analysis
MRI was performed using 1.5-T MRI scanner (Magnetom Aera; Siemens Healthcare, Germany) with an extremity matrix knee coil (a Tim coil). MRI was performed while the patient was in the supine position and a standard 10–15° of knee flexion. The standard knee MRI protocol was the fat-suppressed PD sequence in coronal, axial, and sagittal planes, the T2-weighted sequence in the sagittal plane, and the T1-weighted sequence in the coronal plane.
Statistical analysis
Statistical analysis of the data was performed with the IBM Statistical Package of Social Science (IBM SPSS V26, USA) and MedCalc (Version 19.3.1, USA) package programs at a 95% confidence level. Shapiro-Wilk normality test was used to analyze the distribution of data, and Levene’s test was used to analyze group homogeneity. Continuous variables were presented as mean, standard deviation, and median values, and categorical variables were presented as numbers and percentages. Between MT/LT (<40%, >40%) groups and gender, also with LPTA (≤5°, >5°); The relationship between patellar chondromalacia (yes, no), patellar chondromalacia grade (low grade, high grade), presence of effusion (yes, no), fad-pad edema (yes, no) groups was investigated by Chi-square test.
The relationship between LPTA measurements in patellar chondromalacia grade (low, high), gender (female, male), effusion (yes, no) groups was determined by t-test. Additionally, the relationship between QPA and PPTA measurements in LPTA ≤5°, >5° groups was examined using the Mann-Whitney-U test.
Spearman correlation was used to determine the relationship between LPTA and patellar chondromalacia, QPA, and other variables. LPTA predictive value with the highest sensitivity and specificity for the development of fad-pad edema and ISI predictive values according to patellar tendon length and height were analyzed by ROC curve analysis. P value ≤0.05 was considered statistically significant. P value is a two-sided test.
Results
The study included 277 people (158 women, 119 men). The mean age of the participants was 39.25±11.37 years old. The MT/LT was ≤40 in 41.4 percent of male patients and 58.6 percent of female patients. The mean patellar tendon length, patellar height, TT-TG distance, TGD, MT, and LT of the participant was 41.40±5.94 mm; 41.37±4.56 mm; 10.15±4.02 mm; 7.06±1.69 mm; 13.08±2.73 mm; 23.62±2.93 mm, respectively (Table 1). While the mean LPTA was 11.60°±5.30° in male patients, it was 12.90°±6.41° in female patients. There was no difference in MT/LT ratio and LPTA measurement between the genders of the participants (P=0.510 and P=0.072, respectively).
Table 1
| Measurement | Mean ± SD | Median |
|---|---|---|
| Patellar tendon length (mm) | 41.40±5.94 | 41.3 |
| Patellar height (mm) | 41.37±4.56 | 41.0 |
| Insall-Salvati ratio >1.3 (degrees) | 1.01±0.18 | 1 |
| TT-TG distance (mm) | 10.15±4.02 | 10.5 |
| Patellar angle (degrees) | 122.34±8.50 | 121.8 |
| TSA | 133.20±9.11 | 132.8 |
| TGD (mm) | 7.06±1.69 | 7.1 |
| MT (mm) | 13.08±2.73 | 13 |
| LT (mm) | 23.62±2.93 | 23.6 |
| LPTA (degrees) | 12.34±5.98 | 11.8 |
| PPTA (degrees) | 140.88±7.11 | 1,413 |
| QPA (degrees) | 132.24±8.96 | 1,317 |
| MTI (degrees) | 2,565±604 | 259 |
| LTI (degrees) | 2,478±479 | 246 |
SD, standard deviation; TT-TG, tibial tubercle-trochlear groove; TSA, trochlear sulcus angle; TGD, trochlear groove depth; MT, medial trochlea length; LT, lateral trochlea length; LPTA, lateral patellar tilt angle; PPTA, patella-patellar tendon angle; QPA, quadriceps patellar tendon angle; MTI, medial trochlear inclination; LTI, lateral trochlear inclination.
Thirty-three patients had LPTA ≤5°, and 244 patients had LPTA >5°. Fat-pad edema was present in a total of 73 patients (26.4%). While the most detected subtype of fat-pad edema was located in the suprapatellar (19.9%), we detected the prefemoral type of fat-pad edema the least frequently (0.4%). Patellar chondromalacia was present in 72.9% of all patients. Effusion was present in 92,1% of all patients. While the most detected subtype of effusion was located in the retropatellar region (86.6%), we detected the infrapatellar effusion the least frequently (8.3%) (Table 2). There was no difference between LPTA groups (<5°, >5°) and the presence (P=0.220) and grade (P=0.552) of patellar chondromalacia. There is an insignificant negative correlation between patellar chondromalacia grade and LPTA (r=0.063, P=0.30). There was no difference in the development of effusion in the LPTA groups (>5°, <5°) (P=0.241). Fad-pad edema was found to be significantly higher in the group with LPTA <5° (P=0.046). A low level of significant positive correlation was found between QPA and patellar tendon length. There was no significant correlation between other variables and QPA. There is no difference between QPA and PPTA angles between the groups with LPTA <5° and LPTA >5° (P=0.503, P=0.188). Among the same groups, TT-TG distance was found to be significantly higher in the group with LPTA >5° (P=0.001).
Table 2
| MRI findings | Present, n (%) | Absent, n (%) |
|---|---|---|
| Fat-pad edema (total) | 73 (26.4) | 204 (73.6) |
| SL-Hoffa | 13 (4.7) | 264 (95.3) |
| Non-SL-Hoffa | 17 (6.1) | 260 (93.9) |
| Prefemoral | 1 (0.4) | 276 (99.6) |
| Suprapatellar | 55 (19.9) | 222 (80.1) |
| Patellar hondromalacia | 202 (72.9) | 75 (27.1) |
| Effusion (total) | 255 (92.1) | 22 (7.9) |
| Suprapatellar | 152 (54.9) | 125 (45.1) |
| Retropatellar | 240 (86.6) | 37 (13.4) |
| Infrapatellar | 23 (8.3) | 254 (91.7) |
| Intraarticular (Joint spacing) | 189 (68.2) | 88 (31.8) |
MRI, magnetic resonance imaging; SL-Hoffa, Superolateral Hoffa’s Fat Pad Edema.
TGD and MT were found to be significantly lower in the group with LPTA >5° (P=0.002, P=0.017) (Table 3). There was a positive correlation between patellar tendon length and QPA (P=0.009) (Table 4).
Table 3
| Variables | LPTA ≤5° | LPTA >5° | P value | |||
|---|---|---|---|---|---|---|
| Mean ± SD | Median | Mean ± SD | Median | |||
| Age (years) | 38.88±13.90 | 40.50 | 39.27±11.03 | 40.00 | 0.814 | |
| Patellar tendon length (mm) | 41.47±5.46 | 41.55 | 41.36±6.01 | 41.25 | 0.871 | |
| Patellar height (mm) | 41.76±5.66 | 40.35 | 41.33±4.41 | 41.05 | 0.911 | |
| Insall-Salvati index | 1.00±0.13 | 0.99 | 1.01±0.18 | 1.00 | 0.860 | |
| TT-TG distance (mm) | 7.92±3.39 | 7.50 | 10.44±4.02 | 10.80 | 0.001 | |
| Patella angle (degrees) | 123.45±6.24 | 124.2 | 122.18±8.76 | 121.05 | 0.157 | |
| TSA (mm) | 131.26±8.34 | 130.20 | 133.45±9.21 | 133.05 | 0.210 | |
| TGD (mm) | 7.93±1.75 | 8.02 | 6.95±1.66 | 7.00 | 0.002 | |
| MT (mm) | 14.15±2.84 | 14.10 | 12.94±2.70 | 12.90 | 0.017 | |
| LT (mm) | 23.70±3.16 | 23.20 | 23.63±2.90 | 23.60 | 0.961 | |
| QPA (degrees) | 133.27±8.75 | 132.45 | 132.08±9.01 | 131.30 | 0.503 | |
| MTI (mm) | 24.47±5.13 | 24.75 | 25.82±6.15 | 25.95 | 0.150 | |
| LTI (mm) | 27.75±4.29 | 28.10 | 24.37±4.73 | 24.40 | <0.001 | |
| PPTA (degrees) | 142.11± 6.91 | – | 140.72±7.15 | – | 0.188 | |
LPTA, lateral patellar tilt angle; SD, standard deviation; TT-TG, tibial tubercle-trochlear groove; TSA, trochlear sulcus angle; TGD, trochlear groove depth; MT, medial trochlea length; LT, lateral trochlea length; QPA, quadriceps patellar tendon angle; MTI, medial trochlear inclination; LTI, lateral trochlear inclination; PPTA, patella-patellar tendon angle.
Table 4
| Variables | Quadriceps patellar tendon angle | |
|---|---|---|
| Correlation value | P value | |
| Age | 0.083 | 0.167 |
| Patellar tendon length | 0.156 | 0.009 |
| Patellar height | 0.068 | 0.260 |
| Insall-Salvati index | 0.063 | 0.299 |
| TT-TG distance | −0.103 | 0.087 |
| Patella angle | 0.068 | 0.257 |
| TSA | −0.009 | 0.878 |
| TGD | 0.018 | 0.760 |
| MT | 0.105 | 0.081 |
| LT | 0.030 | 0.622 |
| LPTA | −0.007 | 0.906 |
| MTI | 0.017 | 0.783 |
| LTI | −0.109 | 0.070 |
TT-TG, tibial tubercle-trochlear groove; TSA, trochlear sulcus angle; TGD, trochlear groove depth; MT, medial trochlea length; LT, lateral trochlea length; LPTA, lateral patellar tilt angle; MTI, medial trochlear inclination; LTI, lateral trochlear inclination; PPTA, patella-patellar tendon angle.
In the ROC analysis performed to determine the cut-off value, the LPTA value ≤14.2° which significantly predicted the presence of fad-pad edema, had the highest sensitivity and specificity [sensitivity: 76.71%, specificity: 39.90%, area under the curve (AUC): 0.588, P=0.024] (Figure 3). Patellar tendon length, which significantly predicted the presence of ISI ratio >1.3, was found to be >46.1 mm with the highest sensitivity and specificity (92.31% sensitivity, 84.09% specificity, AUC: 0.888, P<0.001) (Figure 4A). Patellar tendon height, which significantly predicted the presence of ISI >1.3, had the highest sensitivity and specificity of ≤36.1 mm (76.92% sensitivity, 92.05% specificity, AUC: 0.820, P<0.001) (Figure 4B).

Discussion
In this study, fad-pad edema was significantly higher in the patient group with lower LPTA. An LPTA value ≤14.2°, which significantly predicted the presence of fad-pad edema, had the highest sensitivity and specificity. The higher incidence of pathologies such as chondromalacia, fat-pad edema, or effusion in some patients may be related to the difference in the magnitude and the distribution of total transmitted vector forces as a result of these anatomical malalignment (10). Sherman et al. (11) reported that most patellofemoral disorders are the result of bony malalignment. They also added that to achieve a successful treatment process, the bone malalignment should be understood and even the knee arthroplasty shapes to be preferred may change accordingly. Morphological measures and angles described in previous studies vary widely. While many studies report the gender-specific differences in knee anatomy; many studies also opposed this and did not report a statistically significant difference (12-14). Damgacı et al. (6) found that women are more prone to developing bony malalignment, and there was a significant association between patellar malalignment (LPTA and PPTA) and the female gender. In our study, there was no difference in MT/LT ratio (P=0.510) and LPTA (P=0.072) between the genders of the participants.
Patellar tilt is an entity known to be associated with knee pain, and the most practical way of evaluating is LPTA measurement (15). Heesterbeek et al. (16) described that an LPTA >10° has the highest sensitivity and specificity for patellar tilt. Dietrich et al. (17) reported that increased LPTA is a major anatomical risk factor for patellar instability. A normal reference value for LPTA is still not established and remains controversial in the literature data. Many studies argue that LPTA is closely related to pathologies involving the knee joint such as patellofemoral joint degeneration, effusion, and chondromalacia (4,5,18). Cilengir et al. (4) found that patients with trochlear dysplasia, chondromalacia, and quadriceps tendinosis had significantly higher LPTA, and also cases with ≤10° of LPTA is a cut-off value for SL-Hoffa fat pad edema. In several studies, LPTA was lower in patients with chondromalacia. Decreased LPTA may lead to increased patellar compression, resulting in patellar cartilage degeneration (6,19). In our study, a negative correlation between patellar chondromalacia grade and LPTA was found, and also fad-pad edema was significantly higher in the group with LPTA <5°. We found an LPTA cut-off value of ≤14.2° (sensitivity: 76.71%, specificity: 39.90%), which significantly predicted the presence of fad-pad edema. LTI, MTI, and TSA are the measurements for the evaluation of trochlear morphology on the axial MRI. Cilengir et al. (4) revealed that LPTA was negatively correlated with LTI and trochlear dysplasia. TSA is described as the angle between the medial and lateral trochlear facets. Many researchers suggested that an abnormal trochlear morphology can facilitate cartilage defects. It may be caused by abnormal stress on the cartilage due to a flat and shallow trochlea. Trochlear dysplasia was defined as having an LTI of fewer than 11° or an MT/LT ratio of ≤40% or a trochlear sulcus depth of ≤3 mm (4,7-9).
Sagittal plane malalignment is a newly defined entity and is examined with the PPTA (6,20). It has been argued that the narrow PPTA is associated with various knee joint pathologies such as patellar tendinopathy, chondromalacia, and osteoarthritis. An increase in PPTA is described as a positive sagittal patellar tilt and a decrease in PPTA is described as a negative sagittal patellar tilt. An increase in PPTA may lead to volume loss of quadriceps muscle (20).
QPA measurement in this study described by Cilengir et al. (4) for the first time in the literature. QPA is a newly discovered angle showing the axis of the vectorial sum of the forces on the patella. As the QPA changes, the force transmitted to the patella also changes (21). Recently, there are only few studies evaluated the QPA (4,21). For this reason, it has not been fully clarified which measurements are associated with QPA and abnormal QPA values may predispose to which pathologies. Cilengir et al. (4) revealed that QPA is larger in patients with wider trochlear sulcus. Shallow or flat TSA may predispose patellofemoral instability and trochlear dysplasia (22). Wide TSA causes discrepancy as the patella slides over the femoral trochlea, which is the cause of patellofemoral instability (22,23). Quadriceps mechanism is the main tendon system responsible for stabilizing the patella, the angle of junction with the patellar tendon can affect the success of these forces in stabilizing the patella. Cilengir et al. (4) also reported that trochlear dysplasia, fat pad edema and quadriceps tendinosis are more frequently seen in cases with greater QPA. This first study only assessed the relationship between morphological measurement and QPA (4). In our study, we found a positive low-level significant correlation between QPA and patellar tendon length. We did not find a relationship between QPA and chondromalacia, effusion, fad pad edema. QPA is not influenced by both lateral and sagittal patellar tilt. We found no significant changes in LPTA and PPTA as QPA increased. As a diffrent from Cilengir et al. (4), our recent study shown no significant relationship was found between LPTA and QPA.
The second study, Yücel et al. (21) investigated the association between QPA and meniscal injury. They reported that larger QPA is increasing the frequency of total anterior cruciate ligaman tear. However larger QPA did not increase the menisci tear (21). The meniscus distributes the pressure transmitted to the main joint to the knee joint surface and absorbs shock in case of excessive loading. QPA represents the vectorial sum of the forces that support the patella and joint from the anterior during dynamic movement of the knee. As the angle between the tendon of quadriceps and patella increases, the resultant force which stabilizing the knee anteriorly is decreases. Thus, decreased vectorial sum of the forces may cause loading on anterior cruciate ligaman (21).
QPA is a newly defined angle and there are only two studies on it in the literature. For this reason, there is only little data available on it. However, more studies are needed to understand the extent to which it is affected by variations in the knee joint.
TT-TG distance is widely used to measure the risk of patellofemoral instability. In many studies, there are significant differences between the TT-TG distance measured using bone landmarks on CT and the measurements made using cartilage landmarks on MRI (21). It has been argued that measurements made by taking cartilage landmarks as a criterion are more accurate (24). In addition, in many studies, the TT-TG distance was found to be higher in patients with knee pain, and trochlear dysplasia, abnormal patellar height, and TT-TG distance were found among the causes of instability (20,24). While patellar tilt is the most important cause of instability, recent studies have shown that the frequency of patellar height and pathological TT-TG distance is much higher than previously thought (24). Panni et al. (25) reported that trochlear dysplasia is related to the TT-TG measure and LPTA. In our study, TT-TG distance was found to be significantly higher in the group with LPTA >5° (P=0.001). Nakamura et al. (26) reported that increased TT-TG distance is closely correlated to patellar tilt and greater risk of recurrent patellar dislocation in young adults. Abnormal increase in TT-TG distance; it pulls the patella laterally, causing an increase in loading on the lateral compartment of the patella (4).
The current study highlights the complicated association between LPTA, QPA and diverse anatomical parameters within the knee joint, emphasizing the clinical significance of these findings. Notably, the increased incidence of fad-pad edema in patients with LPTA <5 highlights the potential clinical implications of patellar malalignment. The higher TT-TG distance, along with lower TGD and MT in individuals with elevated LPTA, suggests a complicated interaction of factors contributing to patellofemoral joint pathology. Furthermore, the observed positive correlation between QPA and patellar tendon length emphasizes the importance of considering multiple anatomical variables in understanding patellar mechanics. Interestingly, the lack of significant differences in QPA and PPTA between groups with different LPTA implies that other factors may influence these angles, necessitating a comprehensive approach in clinical assessment and management. These findings contribute valuable insights for clinicians in evaluating and addressing patellofemoral disorders, enhancing the understanding of biomechanical complexity involved in knee joint pathophysiology.
Our study has some limitations. The study design was retrospective. Clinical findings, the body mass index, and socioeconomic features of patients were not included in the study. An arthroscopic control did not perform while grading chondromalacia. Chondromalacia was evaluated by MRI only. Our patient population size was limited. In our study, the evaluation was performed by a single radiologist. In a study where the selection of suitable slice was important and the establishing of some points in angle measurements was subjective, the repeatability of the results was not assessed. To minimise this, the operator perform the same measurement more than once. There is no definitive cutoff for the normal LPTA value and we chose 5 based on some publications (4). However, there are also authors in the literature who accept higher and different values for LPTA (27).
Conclusions
Patients with a low LPTA can be more carefully examined for chondromalacia and fad-pad edema in clinical and MRI examination. QPA is independent from many angles of the knee and does not change significantly according to these angles. TT-TG distance was higher, TGD and MT were lower in the group with higher LPTA. Patients with these angle combinations should be carefully evaluated for trochlear dysplasia. Being aware of the morphological malalignment in the knee joint and knowing that they may be associated with underlying pathologies will enable us to better understand the underlying causes of malalignment, instability, and knee pain.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://qims.amegroups.com/article/view/10.21037/qims-23-1592/rc
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://qims.amegroups.com/article/view/10.21037/qims-23-1592/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Ethics committee approval was obtained from a Local Scientific Research Ethics Committee (decision number: 137, date: June 30, 2021). And individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Thomas S, Rupiper D, Stacy GS. Imaging of the patellofemoral joint. Clin Sports Med 2014;33:413-36. [Crossref] [PubMed]
- Asseln M, Hänisch C, Schick F, Radermacher K. Gender differences in knee morphology and the prospects for implant design in total knee replacement. Knee 2018;25:545-58. [Crossref] [PubMed]
- Nacey NC, Geeslin MG, Miller GW, Pierce JL. Magnetic resonance imaging of the knee: An overview and update of conventional and state of the art imaging. J Magn Reson Imaging 2017;45:1257-75. [Crossref] [PubMed]
- Cilengir AH, Cetinoglu YK, Kazimoglu C, Gelal MF, Mete BD, Elmali F, Tosun O. The relationship between patellar tilt and quadriceps patellar tendon angle with anatomical variations and pathologies of the knee joint. Eur J Radiol 2021;139:109719. [Crossref] [PubMed]
- Zikria B, Rinaldi J, Guermazi A, Haj-Mirzaian A, Pishgar F, Roemer FW, Hakky M, Sereni C, Demehri S. Lateral patellar tilt and its longitudinal association with patellofemoral osteoarthritis-related structural damage: Analysis of the osteoarthritis initiative data. Knee 2020;27:1971-9. [Crossref] [PubMed]
- Damgacı L, Özer H, Duran S. Patella-patellar tendon angle and lateral patella-tilt angle decrease patients with chondromalacia patella. Knee Surg Sports Traumatol Arthrosc 2020;28:2715-21. [Crossref] [PubMed]
- McCrum E, Cooper K, Wittstein J, French RJ. Imaging of Patellofemoral Instability. Clin Sports Med 2021;40:693-712. [Crossref] [PubMed]
- Haj-Mirzaian A, Guermazi A, Pishgar F, Roemer FW, Sereni C, Hakky M, Zikria B, Demehri S. Patellofemoral morphology measurements and their associations with tibiofemoral osteoarthritis-related structural damage: exploratory analysis on the osteoarthritis initiative. Eur Radiol 2020;30:128-40. [Crossref] [PubMed]
- Bayhan IA, Kirat A, Alpay Y, Ozkul B, Kargin D. Tibial tubercle-trochlear groove distance and angle are higher in children with patellar instability. Knee Surg Sports Traumatol Arthrosc 2018;26:3566-71. [Crossref] [PubMed]
- Crossley KM, Hinman RS. The patellofemoral joint: the forgotten joint in knee osteoarthritis. Osteoarthritis Cartilage 2011;19:765-7. [Crossref] [PubMed]
- Sherman SL, Plackis AC, Nuelle CW. Patellofemoral anatomy and biomechanics. Clin Sports Med 2014;33:389-401. [Crossref] [PubMed]
- Asseln M, Hänisch C, Schick F, Radermacher K. Gender differences in knee morphology and the prospects for implant design in total knee replacement. Knee 2018;25:545-58. [Crossref] [PubMed]
- Hitt K, Shurman JR 2nd, Greene K, McCarthy J, Moskal J, Hoeman T, Mont MA. Anthropometric measurements of the human knee: correlation to the sizing of current knee arthroplasty systems. J Bone Joint Surg Am 2003;85-A:115-22.
- van den Heever DJ, Scheffer C, Erasmus P, Dillon E. Classification of gender and race in the distal femur using self organising maps. Knee 2012;19:488-92. [Crossref] [PubMed]
- Haj-Mirzaian A, Guermazi A, Hakky M, Sereni C, Zikria B, Roemer FW, Tanaka MJ, Cosgarea AJ, Demehri S. Tibial tuberosity to trochlear groove distance and its association with patellofemoral osteoarthritis-related structural damage worsening: data from the osteoarthritis initiative. Eur Radiol 2018;28:4669-80. [Crossref] [PubMed]
- Heesterbeek PJ, Beumers MP, Jacobs WC, Havinga ME, Wymenga AB. A comparison of reproducibility of measurement techniques for patella position on axial radiographs after total knee arthroplasty. Knee 2007;14:411-6. [Crossref] [PubMed]
- Dietrich TJ, Fucentese SF, Pfirrmann CW. Imaging of Individual Anatomical Risk Factors for Patellar Instability. Semin Musculoskelet Radiol 2016;20:65-73. [Crossref] [PubMed]
- Noehren B, Duncan S, Lattermann C. Radiographic parameters associated with lateral patella degeneration in young patients. Knee Surg Sports Traumatol Arthrosc 2012;20:2385-90. [Crossref] [PubMed]
- Tuna BK, Semiz-Oysu A, Pekar B, Bukte Y, Hayirlioglu A. The association of patellofemoral joint morphology with chondromalacia patella: a quantitative MRI analysis. Clin Imaging 2014;38:495-8. [Crossref] [PubMed]
- Kim YM, Joo YB, Lee WY, Park IY, Park YC. Patella-patellar tendon angle decreases in patients with infrapatellar fat pad syndrome and medial patellar plica syndrome. Knee Surg Sports Traumatol Arthrosc 2020;28:2609-18. [Crossref] [PubMed]
- Oğuzdoğan GY, Arslan FZ. Evaluation of Anatomical Variations with Morphological Measurements and Their Relationship to Meniscal Injury and Ligament Damage. J Knee Surg 2023;36:1357-64. [Crossref] [PubMed]
- Batailler C, Neyret P. Trochlear dysplasia: imaging and treatment options. EFORT Open Rev 2018;3:240-7. [Crossref] [PubMed]
- Duthon VB. Acute traumatic patellar dislocation. Orthop Traumatol Surg Res 2015;101:S59-67. [Crossref] [PubMed]
- Berruto M, Ferrua P, Carimati G, Uboldi F, Gala L. Patellofemoral instability: classification and imaging. Joints 2013;1:7-14.
- Panni AS, Cerciello S, Maffulli N, Di Cesare M, Servien E, Neyret P. Patellar shape can be a predisposing factor in patellar instability. Knee Surg Sports Traumatol Arthrosc 2011;19:663-70. [Crossref] [PubMed]
- Nakamura S, Shima K, Kuriyama S, Nishitani K, Ito H, Matsuda S. Tibial Tubercle-Trochlear Groove Distance Influences Patellar Tilt After Total Knee Arthroplasty. J Arthroplasty 2019;34:3080-7. [Crossref] [PubMed]
- Hochreiter B, Hess S, Moser L, Hirschmann MT, Amsler F, Behrend H. Healthy knees have a highly variable patellofemoral alignment: a systematic review. Knee Surg Sports Traumatol Arthrosc 2020;28:398-406. [Crossref] [PubMed]


