
Incarcerated gravid uterus: an imaging challenge
Introduction
Incarcerated uterus is an uncommon complication of pregnancy which if not recognized and treated promptly can lead to serious adverse outcome. The uterus may be retroverted in about 15% of females before pregnancy and in another 11% during the first trimester of pregnancy (1). The gravid uterus, in most of these patients, spontaneously moves anteriorly and upward by 14–16 weeks gestation. The retroverted gravid uterus remains trapped between the sacral promontory and the pubic symphysis and fails to move upwards in about 1 in 3,000 of these patients, resulting in an incarcerated uterus which puts the mother and fetus at a significant risk for morbidity and mortality (1).
Certain predisposing factors for uterine incarceration include posterior fibroid, endometriosis, adhesive disease [previous surgery, peritonitis, or pelvic inflammatory disease (PID)], variant uterine morphology, deep sacral concavity with a prominent sacral promontory and prior uterine incarceration (1).
The diagnosis of an incarcerated uterus can be missed due to the nonspecific symptoms of dysuria, abdominopelvic pain, vaginal bleeding, back pain and constipation. A high degree of suspicion is therefore very important for a timely diagnosis with urinary retention being a possible indicator that should alert the clinician. On pelvic exam it may present as a large mass in the cul-de-sac with the cervix out of reach of the examining fingers. If the condition goes undiagnosed and therefore untreated it may lead to urinary tract obstruction, urinary tract infection, renal failure, fetal growth restriction, fetal demise, and uterine wall necrosis/rupture (1). Our case is unique as the patient had no symptoms, had no known predisposing factor at the time of presentation, did not have any known complications and delivered a normal healthy male infant near term. The diagnosis of uterine incarceration was missed on the routine second trimester ultrasound (US) and was patient was misdiagnosed as complete placenta previa.
Case presentation
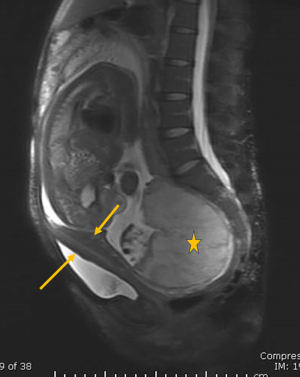
A 28-year-old G1 P0 female presented for a routine anatomy screening US with no reported symptoms or significant past medical or family history. A trans-abdominal US was performed with normal fetal growth and structural survey at 28 weeks of gestation. The placenta was described posterior and completely covering the internal os (Figure 1). A follow up transvaginal US to further assess the placenta and cervix revealed that the cervix was located anterior to the gravid uterus with the uterine fundus with the fundal placenta in the pouch cul-de-sac consistent with incarcerated uterus (Figure 2). Further assessment by magnetic resonance imaging (MRI) revealed an elongated anteriorly displaced cervix (Figure 3). The placenta was fundal and the uterine fundus was located in the cul-de-sac. The lower uterine segment was protruding anteriorly with disproportionately larger growth than the uterine fundus (Figure 4). The urinary bladder was elongated and with a focal ventral outpouching above the pubic symphysis (Figure 4).



The patient was monitored for complications by the maternal fetal medicine (MFM) team. Patient underwent a primary low-transverse cesarean section (PLTCS) at 36 weeks’ gestation delivered a healthy male infant weighing 2,390 grams with APGARs (appearance, pulse, grimace, activity, respiration) of 9/9/9.
Intraoperatively, the uterus was firmly packed to the posterior sacrum and cul-de-sac and the fetus was breech in position. The vesicouterine attachment extended higher (cephalad) than a typical attachment. The wall of the lower anterior uterine segment was thin and could be breached with a blunt finger dissection. A highly prominent sacral promontory and prominent lower lumbar vertebra were noted. At the placenta attachment point, an out-pouching was present resembling a large posterior fibroid. Following the evacuation of the placenta, the out-pouching deflated, and the uterus appeared to be symmetric and relatively normal except for 2 subtle uterine horns near the cornua with a slight midline indention on top of the uterus. These findings possibly suggest a bicornuate.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent for publication of this article and accompanying images was not obtained from the patient or the relatives after all possible attempts were made.
Discussion
Our case highlights that the diagnosis of incarcerated gravid uterus can be challenging and missed as most focus is on intrauterine contents, rather than the adjacent organs and the abdominal wall. The transabdominal US can assess the suprapubic location of the cervix and the bladder just posterior to the anterior abdominal wall. In our case this finding was only seen retrospective to the transvaginal sonogram which revealed the cervix anterior to the uterine fundus in the cul-de-sac. In an incarcerated uterus, the uterine fundus is in the cul-de-sac and can be mistaken as the lower uterine segment. And if the placenta is fundal, the US can be misinterpreted as a placenta previa, as was in our case. The patient was subsequently diagnosed correctly, and the incarcerated uterus was confirmed on MRI of the pelvis. No intervention was contemplated, and the patient delivered a healthy male infant via an elective caesarean section (C section) at 36 weeks.
A retroverted uterus is a relatively common finding in the first trimester of pregnancy affecting 15% of all pregnancies (1). However, by weeks 14 to 16 of gestation the fetus and uterus gradually ascend towards the abdomen, out of the pelvic cavity. When this spontaneous correction fails, incarceration of the uterus develops, in which the gravid uterus is trapped in the posterior pelvic cavity (2,3). The possible etiologies for failure to ascend include fundal fibroid, pelvic adhesions, PID, congenital uterine anomalies, endometriosis, prominent sacral promontory and previous uterine incarceration (1,4). Although there are risk factors associated with the development of an incarcerated uterus, pregnant patients with no apparent risk factors at the time of presentation, such as the patient discussed in our report, made up the largest portion (50%) of those with incarcerated uterus (4). The patient discussed in our case had a few potential risk factors for incarcerated uterus which included a prominent sacral promontory, prominent lower lumbar vertebrae, and possible bicornate uterus. None of these were evident or diagnosed prior to the C section, making our case a unique learning opportunity for having a high degree of clinical suspicion in order to identify them preoperatively.
As stated above, it was the transvaginal sonogram which revealed the correct position of the uterus in this patient. This is a unique elucidation as transabdominal US has been noted to be superior to transvaginal US in identifying the relationships of the pelvic adnexa in relation to the position of the internal ostium of the cervix in previously reported cases of incarcerated uterus (5).
MRI and US are complementary non-invasive modalities for diagnosis of an incarcerated gravid uterus. MRI has an added advantage over US in the complete visualization of the gravid uterus and its relation to adjacent organs due to the large field of view, excellent contrast between the uterus and its adjacent organs and its multi-planar imaging capability. The elongated and anteriorly displaced cervix is the key imaging finding on US and MRI. On US this is seen as two hypo-echogenic layers with an intervening echogenic layer just posterior to the abdominal wall. On MRI it is seen as T2 hypointense linear structure along the anterior aspect of the retroverted uterus. It is frequently elongated and thinned and is parallel to the vagina which differs from the normal appearance of the cervix at a right angle to the vagina. On sagittal T2 sequence retroverted uterus is located deep in the posterior pelvis, below the sacral promontory. There is anterior and superior displacement of the bladder which lies above the pubic symphysis. Ventral out-pouching of the anterior bladder wall can be seen just cranial to the pubic symphysis on mid-sagittal magnetic resonance (MR) images, due to mass effect by the gravid uterus. There is disproportionate growth of the anterior wall of the lower uterine segment leading to sacculation while the fundus of the retroverted gravid uterus remains relatively growth-restricted due to entrapment in the posterior pelvis. In the third trimester, uterine contractions usually fail to dilate the cervix because of incarceration, with a risk of uterine rupture of the thinned lower uterine segment (6).
Most authors recommend restoring uterine polarity by manual reduction, colonoscopic insufflation of the recto-sigmoid or operative reduction via laparoscopy or laparotomy. However, at the time of diagnosis, there had not been a single superior treatment modality for incarnated gravid uterus established, most likely due to the rarity of this obstetric condition (5). Furthermore, as the patient was in their second trimester at the time of diagnosis, the MFM team deemed the risk of possible complications including uterine rupture and/or preterm delivery to be too high to attempt a repositioning of the uterus. This is why a C section was planned and restoring uterine polarity was not known to be attempted. The patient delivered near term by C section without any complications.
A thorough review of adjacent organs is vital, because any sub-umbilical incision may lead to injury to the urinary bladder, the cervix and/or vaginal vault before accessing the posterior uterine wall. Assessment of the position of adjacent organs, with reference to the umbilicus, should guide the surgeon to avoid transection of any other displaced structure.
Important differential diagnosis of an incarcerated gravid uterus includes a fibroid with cystic degeneration (a myometrial mass on US and MRI), uterine torsion (changed position of the placenta/ovarian vessels), uterine anomalies (evaluation of the uterine contour, presence of a separated endometrium) and any pelvic/adnexal mass extending into the cul-de-sac (mass in the Douglas separated from the uterus) (6).
In this report, a nulliparous female presented for a routine pre-natal screen with no complaints or reported symptoms. A transabdominal sonogram initially misdiagnosed this patient with placenta previa at which point the patient was referred to MFM for further management and evaluation. The transvaginal US was the imaging technique which correctly revealed the cervix to be anterior to the uterine fundus in the cul-de-sac. This is a unique elucidation as transabdominal US has been noted in the literature to be superior to transvaginal US in the diagnosis of incarcerated uterus (6).
This case highlighted the complexities of diagnosing the rare obstetric condition of incarcerated uterus especially when no symptoms commonly associated with the condition were reported and no risk factors were known at the time of presentation. Achieving the correct diagnosis is critical to monitor and prevent potentially fatal complications, attempt to restore uterine polarity if appropriate, and to implement the safest delivery modality. Upon performing the C section, it was discovered the patient had prominent lower lumbar vertebrae, a very prominent sacral promontory, as well as a possible bicornate uterus, all of which may have contributed to the patient presentation making this a unique case. Fully elucidating abnormal findings and maintaining a high index of suspicion for incarcerated uterus, even if no symptoms are reported and/or if the patient has no known risk factors at the time of presentation, can help the radiologist reach a correct diagnosis to reduce maternal and fetal morbidity and mortality.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://qims.amegroups.com/article/view/10.21037/qims-23-1399/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent for publication of this article and accompanying images was not obtained from the patient or the relatives after all possible attempts were made.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Gardner CS, Jaffe TA, Hertzberg BS, Javan R, Ho LM. The incarcerated uterus: a review of MRI and ultrasound imaging appearances. AJR Am J Roentgenol 2013;201:223-9. [Crossref] [PubMed]
- Ntafam CN, Beutler BD, Harris RD. Incarcerated gravid uterus: A rare but potentially devastating obstetric complication. Radiol Case Rep 2022;17:1583-6. [Crossref] [PubMed]
- Shnaekel KL, Wendel MP, Rabie NZ, Magann EF. Incarceration of the Gravid Uterus. Obstet Gynecol Surv 2016;71:613-9. [Crossref] [PubMed]
- Kim YS, Kwon BS, Lee YJ. Clinical approach and management of uterine incarceration according to trimester of pregnancy: Case report and literature review. Taiwan J Obstet Gynecol 2021;60:911-5. [Crossref] [PubMed]
- Han C, Wang C, Han L, Liu G, Li H, She F, Xue F, Wang Y. Incarceration of the gravid uterus: a case report and literature review. BMC Pregnancy Childbirth 2019;19:408. [Crossref] [PubMed]
- Dierickx I, Delens F, Backaert T, Pauwels W, Gyselaers W. Case report: incarceration of the gravid uterus: a radiologic and obstetric challenge. J Radiol Case Rep 2014;8:28-36. [Crossref] [PubMed]


