
Preoperative 3-dimensional visualization technology-assisted laparoscopic resection of ectopic pheochromocytoma surrounding the renal artery: a case description
Introduction
Ectopic pheochromocytoma, or paraganglioma (PGL), accounts for approximately 10% of all pheochromocytoma and paraganglioma (PPGL) cases (1). It can occur at various sites and is accompanied by refractory hypertension or a transient hypertensive crisis in some cases. Although more than half of the patients lack specific manifestations owing to the absence of early symptoms, they present with incidentalomas (2) that often involve surrounding tissues or organs (3). Herein, we describe a case of ectopic pheochromocytoma surrounding the right renal artery. Preoperative visualization was achieved via 3-dimensional (3D) reconstruction to evaluate the tumor and surrounding tissues. Subsequently, laparoscopy-assisted resection was performed without causing injury to the renal artery.
Case presentation
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was provided by the patient’s legal guardians for publication of this article and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
A 14-year-old boy presented to the Affiliated Jinhua Hospital, Zhejiang University School of Medicine (Jinhua, China), because of occasional dull flank pain for the past 3 years, which was evident during exercise. There were no positive signs in the abdomen and no history of hypertension.
Computed tomography angiography (CTA) showed a mass with a heterogeneous shadow (5.6×3.6 cm) that was located between the inferior vena cava (IVC) and the abdominal aorta (AA) and enwrapped the right renal artery (Figure 1) without being metastasized. Magnetic resonance imaging (MRI) revealed similar findings. According to the results of blood tests, most hormone levels were normal during endocrinological examination (plasma metanephrine, 35.3 pg/mL; plasma dopamine, <18.0 pg/mL; plasma epinephrine, <24.0 pg/mL; plasma norepinephrine, 210.2 pg/mL; plasma renin, 86.25 uIU/mL; angiotensin II, 91 pg/mL; plasma aldosterone, 258 pg/mL; blood cortisol, 573.14 nmol/L at 8:00 am, 37.76 nmol/L at 0:00 am, and 274.23 nmol/L at 4:00 pm; 24-hour urinary cortisol, 570.27 nmol), whereas plasma normetanephrine were significantly higher (248.9 pg/mL) and adrenocorticotropic hormone (ACTH) level were slightly higher (71.59 pg/mL). Based on these findings, the patient was eventually diagnosed with ectopic pheochromocytoma.

The enhanced computed tomography (CT) and magnetic resonance (MR) Digital Imaging and Communications in Medicine (DICOM) image data were rigidly registered using the 3D Slicer software (https://www.slicer.org/). The “Segment Editor” module was used for 3D reconstruction. The resulting image showed deformation of the IVC due to the compression of the tumor on it, and part of the right renal artery was surrounded by the tumor (Figure 2).

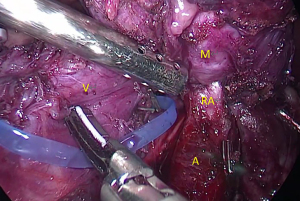
The patient was administered 10 mg phenoxybenzanine hydrochloride orally twice a day for 1 week, followed by peritoneal laparoscopic resection of ectopic pheochromocytoma. Blood volume was expanded through fluid infusion 2 days before surgery to reduce intraoperative fluctuations in blood pressure. Before the surgery, the patient was informed of the possibility of intraoperative vascular injury and intraoperative IVC or right renal artery reconstruction. The patient took a left lateral lying position. The location of the ports were similar to those of conventional laparoscopic adrenalectomy (LA) (10 mm port to the right of the umbilicus was used as the observation hole, 2 operation holes were located at the lower edge of the rib on the right midclavicular line, and the intersection of the line between the observation hole and the umbilicus and the right anterior axillary line). During the surgery, the tumor was found to adhere to the IVC and aorta. In the process of separating the tumor, we found that the blood vessels of the tumor were scattered on the surface of the tumor. We controlled the blood supply of the tumor by separating the exposed blood vessels and cutting them off. After dissecting the lower half of the tumor, we lifted the tumor; it could be observed that the tumor was wrapping around the right renal artery, as shown in the reconstructed image (Figure 3). After careful dissection, the right renal artery surrounded by the tumor was separated without causing vascular wall injury. The surgery was completed in 145 minutes. The intraoperative systolic blood pressure ranged from 96 to 220 mmHg, whereas the diastolic blood pressure ranged from 60 to 130 mmHg. No significant fluctuations in blood pressure were observed postoperatively. Pathological examination revealed characteristics similar to those of pheochromocytoma (Figure 4). The patient was discharged 5 days after surgery, and CT was repeated regularly. No recurrence, metastasis, or other complications were observed after 6 months of follow-up.

Discussion
LA is the gold-standard method for the treatment of most adrenal lesions. However, in cases of large pheochromocytomas (PCC), LA can be extremely challenging owing to limitations such as 2-dimensional (2D) visualization and instability of the camera platform (4). Large adrenal tumors are typically defined as those with a diameter of >5 cm (5). According to Wang et al., tumor size is an independent predictor of a longer surgical time and increased blood loss in large tumors (6). Therefore, a comprehensive preoperative evaluation is particularly important for selecting the optimal surgical plan and controlling surgical risk in patients with large tumors.
In addition to the challenges associated with the tumor size, the varied locations of ectopic pheochromocytoma increase the difficulty of surgery. Many researchers have suggested that preoperative imaging reconstruction enhances the understanding of the retroperitoneal mass and its surrounding anatomical location. Yao et al. found that preoperative stereographic 3D printing models were of great significance when planning the resection of a large PCC/PGL. Specifically, the 3D printing models reduced the operative time and blood loss (7). On comparing differences in the cognition of surgeons on blood vessels, Yang et al. found that 3D printing models improved the understanding of the surgical anatomy of retroperitoneal tumors (8). Although 3D printing models offer convenience for surgery, they are time-consuming and expensive. Some clinical cases of giant ectopic PCC have been reported. These PCC affect the surrounding tissues owing to their excessive size and may invade blood vessels. Wang et al. reported a case of a large PCC adhering closely to the AA and IVC. The AA and IVC were simultaneously removed, and 2 great vessels were reconstructed using 2 externally supported polytetrafluoroethylene (ePTFE) grafts (9). Tumor size is not the only risk factor for pheochromocytoma invading surrounding tissue, Patel et al. described a tumor measured 3.5 cm in diameter and showed evidence of capsular and vascular invasion (10). Preoperative reconstruction image is necessary to provide the surgeon with a 3D perspective and formulate appropriate surgical strategies for ectopic PCC affecting the surrounding tissues and organs. After reviewing articles on adrenal tumor and combining with clinical experience, we recommended 3D reconstruction of adrenal tumor when it is excessively large, has a close relationship with the surrounding organs and blood vessels, or is considered a pheochromocytoma or other hormone-releasing tumor; 3D imaging can help in designing an appropriate approach and avoiding unnecessary tumor extrusion (11,12). In this case study, we used 3D Slicer, a free and open-source software, to visualize and reconstruct the vascular organs surrounding the ectopic pheochromocytoma. After the blood vessels surrounding the tumor were evaluated, a multi-disciplinary treatment (MDT) strategy was implemented in combination with vascular surgery and other related departments including department of anesthesiology and endocrinology before the operation. We planned to separate the right renal artery surrounded by the tumor and be prepared for vascular reconstruction during surgery. The surgery was performed by urologists trained in reconstruction. This treatment strategy neither required specialized equipment nor introduced extra costs. At present, this visualization technique is used in preoperative image reconstruction in many clinical departments, including preoperative visualization of the neurovascular relationship in trigeminal neuralgia (13), visualization of perianal fistulas (14), and mapping of white matter connections in the brain (15).
In this case study, the reconstructed images accurately predicted the events occurring during surgery. The surgeon can see the entire blood vessel through the reconstructed three-dimensional image, the right renal artery has entered the mass which can also be observed in scrolling 2D images, but the 3D image shows that the artery traverses the mass intactly. According to the 3D image, the renal artery was distinguished from the artery of the tumor, and the right renal artery was not mistaken for the artery of the tumor during the operation, which allowed renal artery injury to be avoided. In addition, the tumor needs to be incised when separating the tumor from the renal artery, and the selection of the location of the incision is crucial. We opted to perform tumor insection from the dorsal aspect of renal artery. This decision was based on the observation that this entry point exhibits the shortest distance to the right renal artery and results in a smaller incision wound, thereby minimizing tumor stimulation and reducing intraoperative blood loss. Consequently, we firmly believe that 3D imaging confers significant advantages over 2D imaging when it comes to preoperatively planning optimal tumor incision points and identifying vascular characteristics (their association with tumors). The time and cost of reconstruction were effectively controlled. Recurrence or metastasis was not observed during the 6-month follow-up. Given that guidelines suggest a follow-up of at least 10 years postoperatively, the patient was offered life-long follow-up counseling owing to the intermediate risk of disease (16).
Acknowledgments
Funding: The study was supported by
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://qims.amegroups.com/article/view/10.21037/qims-23-1667/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was provided by the patient’s legal guardians for publication of this article and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Hattori S, Miyajima A, Hirasawa Y, Kikuchi E, Kurihara I, Miyashita K, Shibata H, Nakagawa K, Oya M. Surgical outcome of laparoscopic surgery, including laparoendoscopic single-site surgery, for retroperitoneal paraganglioma compared with adrenal pheochromocytoma. J Endourol 2014;28:686-92. [Crossref] [PubMed]
- Falhammar H, Kjellman M, Calissendorff J. Initial clinical presentation and spectrum of pheochromocytoma: a study of 94 cases from a single center. Endocr Connect 2018;7:186-92. [Crossref] [PubMed]
- Prakobpon T, Santi-Ngamkun A, Usawachintachit M, Ratchanon S, Sowanthip D, Panumatrassamee K. Laparoscopic transperitoneal adrenalectomy in the large adrenal tumor from single center experience. BMC Surg 2021;21:68. [Crossref] [PubMed]
- Gan L, Peng L, Li J, Meng C, Li K, Wu J, Zhang Z, Li Y. Comparison of the effectiveness and safety of robotic-assisted and laparoscopic in adrenalectomy: A systematic review and meta-analysis. Int J Surg 2022;105:106853. [Crossref] [PubMed]
- Cheng Y, Zhu Y. Comparison of Perioperative Outcomes Between Laparoscopic and Robot-Assisted Adrenalectomy for Large Pheochromocytoma (≥ 5cm): A Retrospective Study. Cancer Manag Res 2023;15:1207-16. [Crossref] [PubMed]
- Wang J, Yang B, Sun S, Zhang Y. Perioperative factors influencing the difficulty of retroperitoneal laparoscopic adrenalectomy: a single-center retrospective study. BMC Urol 2022;22:22. [Crossref] [PubMed]
- Yao XW, Ai K, Li Y. Presurgical Planning of 3D Printing for a Large Abdominal Pheochromocytoma and Paraganglioma. Urology 2022;165:356-8. [Crossref] [PubMed]
- Yang T, Lin S, Tan T, Yang J, Pan J, Hu C, Li J, Zou Y. Impact of 3D Printing Technology on Comprehension of Surgical Anatomy of Retroperitoneal Tumor. World J Surg 2018;42:2339-43. [Crossref] [PubMed]
- Wang J, Yuan D, Lu Y, Ma Y, Huang B, Yang Y, Zhao J. A large pheochromocytoma requiring aortic and inferior vena caval reconstruction: A case report. Medicine (Baltimore) 2019;98:e16494. [Crossref] [PubMed]
- Patel T, Singleton LA, Mejia M, Senior A, Millis RM. Pheochromocytoma: A Troublesome Tumor. Cureus 2023;15:e45490. [Crossref] [PubMed]
- Wang X, Zhao Y, Liao Z, Zhang Y. Surgical strategies of complicated pheochromocytomas/paragangliomas and literature review. Front Endocrinol (Lausanne) 2023;14:1129622. [Crossref] [PubMed]
- Kim JH, Lee HC, Kim SJ, Yoon SB, Kong SH, Yu HW, Chai YJ, Choi JY, Lee KE, Lee KW, Min SK, Shin CS, Park KJ. Perioperative hemodynamic instability in pheochromocytoma and sympathetic paraganglioma patients. Sci Rep 2021;11:18574. [Crossref] [PubMed]
- Han KW, Zhang DF, Chen JG, Hou LJ. Presurgical visualization of the neurovascular relationship in trigeminal neuralgia with 3D modeling using free Slicer software. Acta Neurochir (Wien) 2016;158:2195-201. [Crossref] [PubMed]
- Navkar NV, Balakrishnan S, Kharbech S, Sabawi M, Abinahed J, Ahmed A, Al-Ansari A, Omar A, Khanna M, Darweesh A. 3D visualization of perianal fistulas using parametric models. Tech Coloproctol 2022;26:291-300. [Crossref] [PubMed]
- Norton I, Essayed W, Zhang F, Pujol S, Yarmarkovich A, Golby AJ, Kindlmann G, Wassermann D, Estepar RSJ, Rathi Y, Pieper S, Kikinis R, Johnson HJ, Westin CF, O'Donnell LJ. SlicerDMRI: Open Source Diffusion MRI Software for Brain Cancer Research. Cancer Res 2017;77:e101-3. [Crossref] [PubMed]
- Plouin PF, Amar L, Dekkers OM, Fassnacht M, Gimenez-Roqueplo AP, Lenders JW, Lussey-Lepoutre C, Steichen OGuideline Working Group. European Society of Endocrinology Clinical Practice Guideline for long-term follow-up of patients operated on for a phaeochromocytoma or a paraganglioma. Eur J Endocrinol 2016;174:G1-G10. [Crossref] [PubMed]


