
Ultrasound-guided acupotomy release for treating common peroneal nerve entrapment syndrome: a case description
Introduction
In China, some doctors have adopted the method of using acupotomy to dissect the fibular tunnel in treating common peroneal nerve entrapment syndrome (CPNES) (1). Acupotomy is a procedure that combines traditional Chinese acupuncture needles and scalpels and is thus also referred to as needle-knife therapy. Acupotomy can cut and detach the abnormal, cicatricial, and contractured tissues by only causing microtrauma. Acupotomy is mainly used to treat chronic injuries of the motor system, cervical and lumbar diseases, and degenerative diseases or pathologies of the bones and joints, such as tenosynovitis, muscle injury, periarthritis of the shoulder, cervical spondylosis, lumbar disc herniation, knee osteoarthritis, and heel pain, among others (2-4). However, with blind operation, it is more likely that nerves and blood vessels will be damaged, and it is difficult to control the depth and direction of needle insertion. From February to March 2023, to improve the accuracy and safety of treatment, we used ultrasound guidance to dissect the peroneus longus muscle and nearby fascial tissue.
Here, we describe a patient with CPNES who was successfully treated by releasing the tension of the peroneus longus muscle using acupotomy under ultrasound guidance. We focus on the application of ultrasound anatomic images and clinical treatment. To our knowledge, this technique has not been previously reported.
Case presentation
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this article and accompanying images. A copy of the written consent is available for review by the editorial office of this journal. A 68-year-old male patient experienced continuous numbness and a sensation of heaviness, similar to being weighed down by a sandbag, in the lateral area of his right lower leg lasting over a decade. At the initial diagnosis, he had completely lost his two-point discrimination, but the pain was not significant. After walking 5,000–6,000 steps, the heaviness in his right leg significantly increased, which limited his ability to walk. The patient had not received any treatment or other therapies for the leg symptoms before this treatment. The patient had been diagnosed with diabetes over a decade prior and, at the time of admission, was taking 0.1 g of acarbose twice daily with meals and 0.5 g of metformin once daily. We considered that diabetes over the years had led to neuroedema, which in turn caused the compression of the common peroneal nerve due to the relative stenosis of the fibular canal.
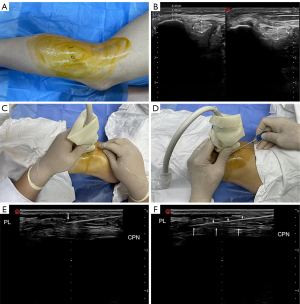
A Labat ultrasonic linear array probe (Winsonic, Shenzhen, China) was used to examine the patient. The patient lay on the surgical bed on his side, and the operating area was completely exposed. First, the surgeon located the head of the fibula, marked its position with a marker pen, and sketched out the course of the common peroneal nerve about 2 cm below it (Figure 1A). Before the surgery, a comparison was made under ultrasound between the cross-sectional area of the common peroneal nerve on the healthy side and the affected side. The results showed that the cross-sectional area of the common peroneal nerve on the affected side was larger than that on the healthy side (Figure 1B). Then, the operative area was disinfected with iodine, and the ultrasound probe was wrapped in a sterile protective cover. First, the ultrasound probe was swept along the transverse axis of the common peroneal nerve. Second, according to the cross method, the probe was rotated 90º to ensure that the common peroneal nerve was consistently within the field of view, with the marked point of the probe facing the distal end and showing the longitudinal axis image of the common peroneal nerve. Under ultrasound guidance, local anesthesia was administered layer by layer using a disposable sterile syringe with a needle (5 mL; BD Biosciences, Beijing, China) injecting 2 mL of 2% lidocaine solution (Figure 1C). The common peroneal nerve crosses over the lateral head of the gastrocnemius muscle and enters the peroneus longus muscle, coursing between the surface of the fibula and the peroneus longus muscle, forming a pathway known as the fibular canal (5). A needle knife 2.0 mm × 50 mm in size (LaoZongYi, Ji’an, China) was chosen to make an incision at the proximal end of the probe, parallel to the course of the common peroneal nerve. The peroneus longus muscle was dissected and loosened down to the surface of the common peroneal nerve, and the soft tissue located between the medial edge of the fibularis muscle and the entrance of the fibular canal was freed (Figure 1D-1F). The needle knife was used to make four to five repeated incisions before being withdrawn. Treatment was administered once a week for 5 weeks.
After five treatments, the heaviness and numbness in the patient’s right leg were greatly relieved, and the two-point discrimination was essentially recovered. Before treatment, the two-point discrimination had been completely lost due to obvious sensory abnormalities, and after treatment, the two-point discrimination was 25 mm. Two months after the final treatment, the patient’s condition was stable during follow-up, and there was no recurrence. Two months after the operation, the patient was able to walk 15,000 steps daily without any significant abnormalities in his right leg. His quality of life has greatly improved.
Patient perspective
We contacted this patient in May 2023 and asked him for his views on our therapy. No complaints or questions were expressed. Before the therapy, this patient experienced heaviness and numbness of the right lower leg. After the therapy, the symptoms of heaviness and numbness were significantly relieved. He felt the therapy was successful.
Discussion
CPNES is the most common nerve entrapment syndrome of the lower limbs (6). Multiple factors can cause damage to the common peroneal nerve, among which entrapment is the most prevalent, typically occurring at the fibular neck. The main feature of CPNES in clinical practice is numbness in the lower limb, extending from the anterolateral aspect of the leg from just below the fibular canal to the dorsal aspect of the foot, and symptoms of foot drop may also occur. Treatment options for CPNES vary depending on the underlying cause. If the nerve damage results from traumatic injury, such as a car accident, gunshot, or sharp instrument damage, or from continuous damage after knee replacement or dislocation surgery, nerve or tendon transplantation may be necessary (7). Autologous nerve transplantation is the preferred method although some experts recommend performing both nerve and tendon transplantation concurrently due to the poor prognosis of nerve transplantation alone (8). If the condition arises from ankle sprains or metabolic diseases such as diabetes, as in this case, peripheral nerve decompression surgery can be considered. Studies have shown that patients with diabetes are more likely to develop peroneal neuropathy at the fibular head (9). If there is no occupant lesion, such as a tumor, decompression can be performed using a needle knife, which can reduce the pressure inside the fibular canal, restore nerve circulation, and eliminate nerve edema.
In the past, when performing a downward needle knife operation under blind conditions, there was a danger of damaging the common peroneal nerve, and therefore the needle was often inserted next to the nerve to loosen the entrance of the peroneal canal. Currently, with ultrasound guidance, the nerve surface can be directly loosened.
Compared with peripheral nerve decompression surgery, the needle-knife procedure has the advantages of minimal trauma, fast recovery, and lower costs during the process of releasing the common peroneal nerve. However, the release may not be as thorough as that of surgery; therefore, the needle-knife technique is more suitable for patients with mild-to-moderate nerve compression, as was the case for the patient in this report. With the continuous advancement of modern medicine, visualization technology will become increasingly integrated into clinical procedures.
The limitation of this case report is that acupotomy cannot be applied to particularly severe peroneal nerve injury. When the surgical indication is clear, such as when foot drop has already occurred, immediate surgery may be a better choice.
This case report supports the clinical feasibility of using ultrasound-guided needle-knife surgery to release the common peroneal nerve. Based on this report, relevant basic research and randomized controlled trials can be conducted in the future.
Conclusions
Ultrasound-guided acupotomy release treatment for CPNES is a safe and effective treatment method that can achieve good therapeutic effects with minimal patient trauma and reduced treatment costs compared with previous techniques.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://qims.amegroups.com/article/view/10.21037/qims-23-1277/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this article and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Ren SJ, Wang LF. Observation of Needle-knife in Treatment of Common Peroneal Nerve Entrapment Syndrome. Chinese Journal of Traditional Medical Traumatology & Orthopedics 2020;28:28-30.
- Zhu X, Shen Y, Liu Z, et al. Ultrasound-Guided Percutaneous Release Procedures in the Lumbar Ligamentum Flavum by Acupotomy: A Cadaveric study. Evid Based Complement Alternat Med. 2019;2019:2807901. [Crossref] [PubMed]
- Qiu Z, Li H, Shen Y, et al. Safety and efficacy of ultrasound-guided percutaneous A1 pulley release using a needle knife: An anatomical study. Front Surg 2022;9:967400. [Crossref] [PubMed]
- Zhou Q, Shen Y, Zhu X, et al. Ultrasound-guided percutaneous release procedures in the transverse carpal ligament by acupotomy: A cadaveric study. Front Surg 2022;9:906109. [Crossref] [PubMed]
- Watabe LT, Santos PVBD, Mendes FA, et al. Fibular Nerve Repair by Lateral Sural Cutaneous Nerve Graft: Anatomic Feasibility Study and Clinical Results. World Neurosurg 2021;146:e537-43. [Crossref] [PubMed]
- Poage C, Roth C, Scott B. Peroneal Nerve Palsy: Evaluation and Management. J Am Acad Orthop Surg 2016;24:1-10. [Crossref] [PubMed]
- Park JS, Casale MJ. Posterior Tibial Tendon Transfer for Common Peroneal Nerve Injury. Clin Sports Med 2020;39:819-28. [Crossref] [PubMed]
- Garozzo D, Ferraresi S, Buffatti P. Common peroneal nerve injuries in knee dislocations: results with one-stage nerve repair and tibialis posterior tendon transfer. J Orthop Traumatol 2002;2:135-7. [Crossref] [PubMed]
- Stamboulis E, Vassilopoulos D, Kalfakis N. Symptomatic focal mononeuropathies in diabetic patients: increased or not? J Neurol 2005;252:448-52. [Crossref] [PubMed]


