
Endplatitis short vertebrae
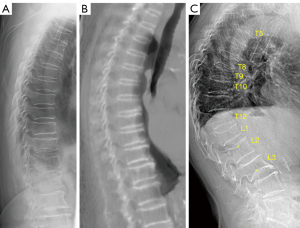
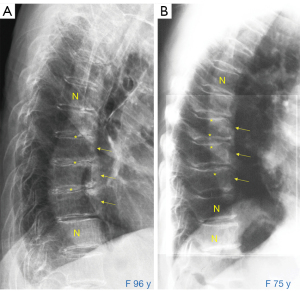
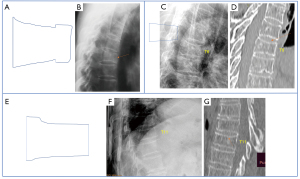
Short vertebrae of acquired cause (SVa) have been defined as the vertebral deformity with decreased vertebral anterior and middle heights, while without apparent anterior wedging or apparent bi-concave changes, i.e., middle height and anterior height are reduced to a similar extent, and without apparent radiographic endplate fracture (1-3). When diagnosing SVa, at least two adjacent short vertebrae (SV) in the same subject are required (1,3). SVa is a mimic of osteoporotic-like vertebral fracture (OLVF). The differentiation of multiple SVa from multiple OLVF is that, multiple SVa appear similar in appearance, while multiple OLVFs commonly have different shapes and different severity (Figure 1). Figure 1A also demonstrates that even when many SVa are already quite severe, they do not apparently ‘fracture’. In our osteoporotic fractures in men (MrOS) and women (MsOS) (Hong Kong) year-18 follow-up study (3,4), we noted that 14.2% of the older men (total n=155; mean age: 87.4 years) and 8.6% of the older women (total n=197; mean age: 85.2 years) had SVa. In a chest radiograph study with subjects of assumed normal bone strength, among in total of 449 men and women aged ≤34 years, no single case had SVa noted (5). In that study, for 66 women aged between 45 and 59 years (mean age: 50.0 years), only 1 case (1.5%) had SVa; whereas for 96 men aged between 45 and 67 years (mean: 54.1 years) and of them substantial portion had physical labor history, 15 cases (15.6%) had SVa. The opposite of OLVF, SVa prevalence tends to be higher among older men than among older women (4,5). In two radiographic studies focused on thoracic and thoracolumbar junction (unpublished data), SVa among Thais was for men 12.9% (26/202; mean age: 73.7 years) and for women 6.6% (13/196; mean age: 73.6 years), SVa among Indonesians was for men 11.5% (20/174; mean age: 70.2 years) and for women 10.3% (24/234; mean age: 70.4 years). In a study focused on the thoracic and thoracolumbar junction, SVa among Italian Caucasian women was 8.4% (24/287; mean age: 73.6 years) (6). Therefore, SVa are uncommon among young subjects, and relatively common among older populations, and SVa may have similar prevalence among East/Southeast Asians and Caucasians. Physical labor could be associated with an increased prevalence of SVa (3,5).
In a cross-sectional study (1), we observed that OLVF is commonly associated with endplate depression, while SVa is not associated with endplate depression. In one longitudinal follow-up study of ours (4), we observed that, while OLVF is associated with an increased risk of further fracture, SVa is not associated with an increased risk of further fracture.
In this letter, we propose that SVa can be classified to at least two categories: (I) those due to low bone mineral density (BMD; or low bone strength, osteopenia/osteoporosis) and (II) those due to endplatitis.
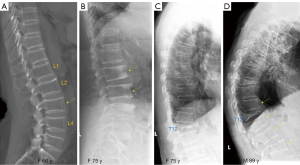
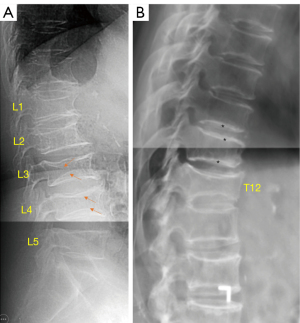
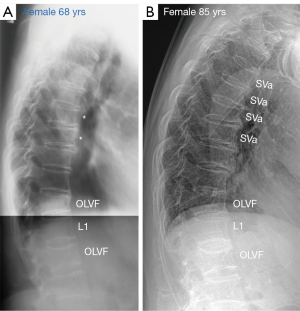
For the vertebral bodies, lower BMD is associated with a decrease of height, but no change in anterior-posterior dimension, leading to an increased biconcavity index and an overall decrease in vertebral body volume (7). For the discs, lower BMD is associated with an increase in disc middle height and the disc biconvexity index is increased (7). Following this, it can be inferred that, without apparent fracture, in patients with low BMD or osteoporosis, low BMD can cause vertebrae to demonstrate SVa appearance (to various degrees). Examples of four cases of assumed low BMD SVa are shown in Figure 2. Low BMD SVa may be associated with intervertebral disc space widening (7,8), without endplate sclerosis, and without osteophyte.
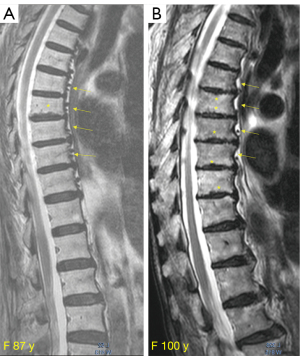
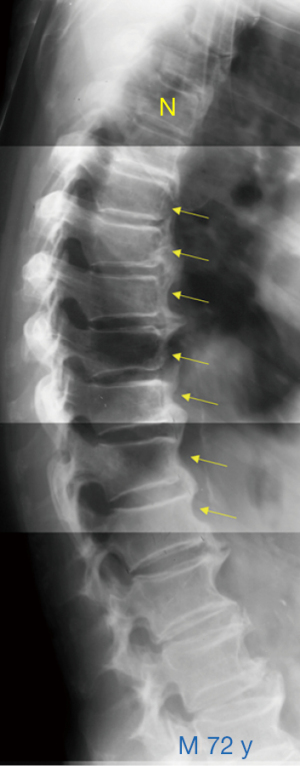
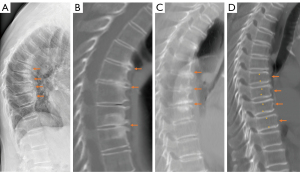
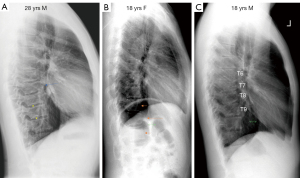
Importantly, one common cause of SVa appears to be endplatitis (1,3). In some cases, both endplatitis and SVa can be simultaneously detected with in-vivo imaging. Figure 3 shows two cases with magnetic resonance imaging (MRI) appearance of endplatitis and associated SVa. Figure 4 shows four cases with computed tomography (CT) appearance of endplatitis and associated SVa. Figure 5 shows two cases with radiographic appearance of endplatitis and associated SVa. Endplatitis SVa is associated with endplate sclerosis and endplate thickening, and maybe associated with intervertebral disc space narrowing, and maybe with vertebral osteophyte. In addition, sometimes, on sagittal image, the anterior upper corner and anterior lower corner of the involved vertebra may become more ‘round-shaped’ (Figure 4B,4C).
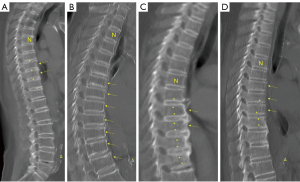
On imaging appearance, the differentiation of low BMD SVa and endplatitis SVa mainly relies on the detection of endplate changes of increased density (on radiograph and CT) and irregular border of the endplate. In our experience, endplatitis SVa is more commonly seen at the thoracic spine and thoracolumbar junction, whereas low BMD SVa is most apparent in the lumbar spine. The distribution of low BMD SVa commonly involves many vertebrae while endplatitis SVa can be relatively more localized (Figure 6). In practice, both radiograph and conventional MRI are not sensitive for the detection of endplatitis. The differentiation between low BMD SVa and endplatitis SVa may not be easy, particularly when only radiograph is available (Figure 7). It can be anticipated that in many cases, these two etiologies can co-exist. Thus, often only SVa can be diagnosed, while the cause of acquired SV cannot always be confirmed by in-vivo imaging.
The relative prevalence of low BMD SVa and endplatitis SVa may depend on the study population. Without solid supporting data, we empirically feel that endplatitis SVa may be more common, particularly among older men. Weight-bearing physical labor may increase the prevalence of endplatitis SVa (3,5). Again, in many cases, these two etiologies can co-exist. In our MrOS and MsOS (Hong Kong) year-18 follow-up study, we reported somewhat mixed results for SVa. On one side, both for males and females, a lower mean BMD was noted for subjects with SVa than those without SVa (4). SVa were also associated with a higher prevalence of other OLVFs (4), probably due to that both low energy trauma and weakened bone quality may facilitate the development of SVa. On the other hand, SVa is not associated with increased fracture risk for other vertebrae (4). The discussion in this letter may help to explain this confusion, as SVa might have contained both low BMD SVa and endplatitis SVa in that study.
Another entity related to endplatitis SVa is osteoarthritic (OA) wedging. SVa and OA wedging share a number of similar features. OA wedging is also without apparent endplate depression and is not associated with an increased further vertebral fracture risk (9). Both OA wedging and SVa tend to involve multiple adjacent vertebrae being similarly deformed, while milder fractural deformities tend more often to be singular with a distinct loss of expected shape (i.e., not multiple adjacent vertebrae appearing similarly deformed). OA wedging is associated with osteophyte formation and intervertebral disc space narrowing (Figure 8). SVa is less commonly associated with osteophyte (though SVa can associate with osteophyte formation). SVa can be without intervertebral disc space narrowing or can be with intervertebral disc space widening, so that the involved vertebrae appear anteroposteriorly ‘elongated’ (Figure 1). OA features in OA wedging more involve the anterior portion of the endplate, while endplatitis in SVa tends to equally involve the anterior portion and posterior portion of endplates (Figure 8). OA wedging is uncommon among East and Southeast Asians, but relatively common among Italian Caucasian older women (around 1% for Chinese and Thais, and 7% for Italian women, mean age of around 75 years) [(6) and unpublished data].
For the radiographic diagnosis of SVa, we commonly require at least two adjacent vertebrae involved. In one study, we demonstrated that SVa-shaped singular vertebral deformity is often associated with CT endplate fracture thus likely to be OLVF, while multiple adjacent SVa are without CT endplate fracture and are likely due to endplatitis (1). Moreover, since the appearance of OLVF can be an anterior wedging or a ‘mixed shape’ (2), then the intermediate shape of anterior wedging and a ‘mixed shape’ will look like an SVa (Figure 9). In addition, it appears that multiple SVa do not start from a distinct apparent singular SV, and then progress to multiple SVa. Instead, multiple SVa start from multiple ‘slight degree’ SVa, and then these SVa progress further in number and severity (Figure 10). Overall, we consider that a singular radiographically SVa-shaped vertebra favors the diagnosis of OLVF, but the diagnosis would be based on statistical probability rather than being an absolute diagnosis. The diagnosis is easier when the extent of deformities is more severe. SVa commonly starts with the reduction of middle and anterior heights. Though biomechanically the posterior part of vertebral body is better supported by vertebral posterior elements, in more severe cases, vertebral posterior height can also be reduced (Figure 6A).
We did not discuss the etiology of endplatitis in this letter as till now we do not have sufficient data for this, particularly we did not have surgical or biopsy histology data. However, we consider the endplatitis discussed in this letter mostly do not fall into the category of classical clinical infection; considering these points: (I) endplatitis prevalence is very low among young and middle-aged populations, and then quickly increases among older populations (5,6); (II) different ethnic groups appeared to have similar prevalences, and with the prevalence consistently higher among men than among women; (III) the vertebral level distribution can be wide (if the etiology is infectious, then the vertebral level distribution may be more localized). However, subclinical infections in disc disorders have been noted to be common, and many pathogens have been identified in MRI normal discs (10,11). Oral antibiotic treatment has been shown to be effective in treating MRI Modic type 1 changes (12,13). More studies on endplatitis SVa potential infectious etiology should be conducted.
SV of developmental cause (SVd; i.e., congenital SV) is very different from SVa. SVd often has other associated changes of adjacent vertebrae (Figure 11), and mostly can be easily differentiated from SVa by an experienced reader. Among older subjects, compared with SVa, SVd is much less common.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: The author has completed the ICMJE uniform disclosure form (available at https://qims.amegroups.com/article/view/10.21037/qims-24-20/coif). Y.X.J.W. serves as the Editor-in-Chief of Quantitative Imaging in Medicine and Surgery. Y.X.J.W. is a co-developer of the ‘CT multi-slice slab reconstruction’ method used in this study to visualize the endplate changes. The author has no other conflicts of interest to declare.
Ethical Statement: The author is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Du EZ, Wáng YXJ. CT detects more osteoporotic endplate depressions than radiograph: a descriptive comparison of 76 vertebrae. Osteoporos Int 2022;33:1569-77. [Crossref] [PubMed]
- Wáng YXJ. An update of our understanding of radiographic diagnostics for prevalent osteoporotic vertebral fracture in elderly women. Quant Imaging Med Surg 2022;12:3495-514. [Crossref] [PubMed]
- Wáng YXJ. A summary of our recent evidence-based works on radiographic diagnostics of prevalent osteoporotic vertebral fracture in older men and women. Quant Imaging Med Surg 2023;13:1264-85. [Crossref] [PubMed]
- Wáng YXJ, Lu ZH, Leung JCS, Fang ZY, Kwok TCY. Osteoporotic-like vertebral fracture with less than 20% height loss is associated with increased further vertebral fracture risk in older women: the MrOS and MsOS (Hong Kong) year-18 follow-up radiograph results. Quant Imaging Med Surg 2023;13:1115-25. [Crossref] [PubMed]
- Ma JB, Wáng YXJ. Chest radiograph prevalence of vertebral deformity among young and middle-aged population of mixed city dwellers and rural residents. J Thorac Dis 2022;14:4685-98. [Crossref] [PubMed]
- Wáng YXJ, Diacinti D, Iannacone A, Kripa E, Leung JCS, Kwok TCY, Diacinti D. A comparison of radiographic degeneration features of older Chinese women and older Italian Caucasian women with a focus on thoracic spine. Aging Clin Exp Res 2023;35:2583-91. [Crossref] [PubMed]
- Kwok AW, Wang YX, Griffith JF, Deng M, Leung JC, Ahuja AT, Leung PC. Morphological changes of lumbar vertebral bodies and intervertebral discs associated with decrease in bone mineral density of the spine: a cross-sectional study in elderly subjects. Spine (Phila Pa 1976) 2012;37:E1415-21. [Crossref] [PubMed]
- Wáng YXJ. Senile osteoporosis is associated with disc degeneration. Quant Imaging Med Surg 2018;8:551-6. [Crossref] [PubMed]
- Abdel-Hamid Osman A, Bassiouni H, Koutri R, Nijs J, Geusens P, Dequeker J. Aging of the thoracic spine: distinction between wedging in osteoarthritis and fracture in osteoporosis--a cross-sectional and longitudinal study. Bone 1994;15:437-42. [Crossref] [PubMed]
- Capoor MN, Ruzicka F, Machackova T, Jancalek R, Smrcka M, Schmitz JE, et al. Prevalence of Propionibacterium acnes in Intervertebral Discs of Patients Undergoing Lumbar Microdiscectomy: A Prospective Cross-Sectional Study. PLoS One 2016;11:e0161676. [Crossref] [PubMed]
- Rajasekaran S, Soundararajan DCR, Tangavel C, Muthurajan R, Sri Vijay Anand KS, Matchado MS, Nayagam SM, Shetty AP, Kanna RM, Dharmalingam K. Human intervertebral discs harbour a unique microbiome and dysbiosis determines health and disease. Eur Spine J 2020;29:1621-40. [Crossref] [PubMed]
- Albert HB, Sorensen JS, Christensen BS, Manniche C. Antibiotic treatment in patients with chronic low back pain and vertebral bone edema (Modic type 1 changes): a double-blind randomized clinical controlled trial of efficacy. Eur Spine J 2013;22:697-707. [Crossref] [PubMed]
- Manniche C, Hall GM. Chronic low back pain, Modic changes and low-grade virulent infection: efficacy of antibiotic treatment. Future Sci OA 2021;7:FSO703. [Crossref] [PubMed]
- Wáng YXJ. Schmorl's node of primarily developmental cause and Schmorl's node of primarily acquired cause: two related yet different entities. Quant Imaging Med Surg 2023;13:4044-9. [Crossref] [PubMed]


