
Ventricular dysfunction consequences of mechanical dyssynchrony in isolated complete right bundle branch block versus left bundle branch block
Introduction
Complete bundle branch block is often associated with underlying cardiovascular abnormalities, such as myocardial infarction, hypertension, or cardiomyopathy (1,2), but it can also occur in individuals without any evidence of other heart diseases, which is called isolated complete bundle branch block. Isolated complete right bundle branch block (CRBBB) and complete left bundle branch block (CLBBB) have a prevalence of 0.18% and 0.1%, respectively, in the general population (3). Isolated CLBBB is correlated with ventricular dysfunction secondary to cardiac contractile dyssynchrony (4-6); however, there are few studies on cardiac mechanical dyssynchrony and ventricular function in isolated CRBBB.
CRBBB leads to delayed depolarization of the regional right ventricle (7) and prolongation of total right ventricular (RV) activation, resulting in a late opening of the pulmonary valve and late RV ejection (8), which may affect mechanical synchrony and ventricular function in isolated CRBBB patients. Isolated CRBBB is generally considered benign with a favorable prognosis (9,10), but several recent investigations have shown that isolated CRBBB is associated with adverse cardiovascular outcomes (11,12). Evidence on cardiac synchrony and ventricular function in isolated CRBBB patients and differences in synchrony and function between isolated CRBBB and CLBBB patients remains inconclusive.
Therefore, this study aimed to: (I) compare cardiac synchrony and systolic and diastolic function in isolated CRBBB patients and healthy subjects; (II) analyze the possible factors associated with ventricular function in isolated CRBBB patients; and (III) compare the different effects of isolated CRBBB patients and isolated CLBBB patients on cardiac synchrony and ventricular systolic and diastolic function. We present this article in accordance with the STROBE reporting checklist (available at https://qims.amegroups.com/article/view/10.21037/qims-23-959/rc).
Methods
Study population
A total of 44 patients with isolated CRBBB who underwent regular annual checkups at the medical examination center of The First Hospital of China Medical University between March 2020 and June 2021 were enrolled in this cross-sectional study. To be eligible for inclusion in this study, the patients had to meet the following inclusion criterion: have a diagnosis of CRBBB on a standard 12-lead electrocardiogram (ECG) without other evidence of heart disease. Patients were excluded from the study if they met any of the following exclusion criteria: (I) had any structural heart disease, such as any valvular dysfunction, congenital heart disease, restrictive, hypertrophic, or dilated cardiomyopathy, ischemic heart disease, myocarditis, pericardial effusion, other supraventricular or ventricular arrhythmias, atrial fibrillation, paced rhythms, or left ventricular ejection fraction (LVEF) <52% in men or <54% in women (13); (II) had any history of coronary artery disease, which was defined as a history of chronic stable angina, unstable angina, non-segment between the S-wave end and the T-wave onset (ST-segment) elevation myocardial infarction or ST-segment elevation acute myocardial infarction, or positive results on an exercise stress test; (III) had any severe systemic disease, including anemia, tumors, infection, hepatorenal insufficiency, and autoimmune disease; (IV) had hypertension, diabetes, hyperlipidemia, hyperthyroidism, hypothyroidism, or pulmonary hypertension; and/or (V) had poor ECG images or poor echocardiographic images with artifacts that led to the failure of the imaging analysis.
In addition, 44 patients who were diagnosed with isolated CLBBB on standard 12-lead ECG and 42 healthy subjects with sinus rhythm were enrolled during the same study period; the exclusion criteria were the same as those for the isolated CRBBB patients. A flow chart of the selection process for the study group is provided in Figure 1.

The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013) and approved by the Ethics Committee of Medical Science Research of The First Hospital of China Medical University (No. 2019-93-2). Informed consent was obtained from all individual participants.
Electrocardiography
Each baseline standard 12-lead ECG was recorded in the supine position at a paper speed of 25 mm/s and calibration of 10 mm/mV using a MAC 5500 ECG machine (GE Healthcare, Waukesha, WI, USA).
CRBBB was defined by baseline standard supine 12-lead ECG findings of: (I) time interval between the Q-wave onset and the S-wave end (QRS duration) ≥120 ms; (II) rsr′, rsR′, or rSR′ in leads V1 or V2; (III) S-wave duration >40 ms or greater than R wave duration in leads I and V6; and (IV) R wave peak time >50 ms in lead V1 but normal values in leads V5 and V6. Of the above criteria, the first three had to be present to make a diagnosis of CRBBB. When a pure dominant R wave with or without a notch was present in V1, criterion IV should be considered met (14).
CLBBB was defined as: (I) QRS duration ≥140 ms in men or ≥130 ms in women; (II) QS or rS in leads V1 and V2; and (III) mid-QRS complex slurring or notching in ≥2 of leads V1, V2, V5, V6, I, and aVL (15).
Echocardiography
Echocardiography was performed within 24 hours of ECG using a Vivid E9 ultrasound system (GE Healthcare) equipped with a 2–4 MHz phased-array probe. Images were acquired with the patient in the left decubitus position during normal respiration and caution was paid to minimize artifacts. At least three consecutive cardiac cycles were stored in the cineloop format for offline analysis using an EchoPAC workstation (GE Healthcare). Two experienced cardiologists with more than 5 years of expertise were blinded to the clinical data and performed the measurements as recommended by the American Society of Echocardiography (ASE) (13).
Assessment of cardiac dyssynchrony
The atrioventricular dyssynchrony parameter was defined as the ratio of the LV diastolic filling time to the RR interval (LVDFT/RR) measured by tissue Doppler imaging, while the interventricular dyssynchrony parameter was defined as interventricular mechanical delay (IVMD) calculated as the difference between the aortic and pulmonary pre-ejection time (16,17).
Right intraventricular synchrony was evaluated by the mechanical dispersion of the right ventricle (MD-RV), which was calculated as the standard deviation of time to the peak longitudinal strain of six segments for the right ventricle based on the peak of the averaged curve by two-dimensional speckle tracking echocardiography (2D-STE) from the RV-focused apical four-chamber view. Left intraventricular synchrony was evaluated by the mechanical dispersion of the left ventricle (MD-LV), which was calculated as the standard deviation of the time to the peak longitudinal strain of 18 segments of the left ventricle from apical four-, two-, and three-chamber views focused on the left ventricle (18,19).
Assessment of RV function
According to the ASE recommendations (20), the RV basal diameter (RV-base), RV mid-diameter (RV-mid), and RV longitudinal dimension (RVLD) were measured to assess RV size. To assess RV systolic function, RV fractional area change (RV-FAC), tricuspid annular plane systolic excursion (TAPSE), systolic velocity of the septal tricuspid annulus (TV-s'), and RV global longitudinal strain (RV GLS) were measured. RV GLS was determined based on the peak of the averaged curve of a six-segment RV model by 2D-STE in the RV-focused apical four-chamber view, and the lower limit of normality was −20.0% for men and −20.3% for women (21).
For RV diastolic function, the ratio of the peak early diastolic tricuspid flow velocity to the peak late tricuspid diastolic flow velocity (RV-E/A), ratio of the peak early diastolic tricuspid flow velocity to the peak early diastolic velocity of the lateral tricuspid annulus (TV-E/e′), and deceleration time of the peak early diastolic tricuspid flow velocity (TV-EDT) were assessed. The RV index of myocardial performance (RV-Tei-Index) was used to evaluate RV global function.
Assessment of LV function
To assess LV systolic function, LV end-diastolic diameter (LVEDD), LV end-diastolic volume (LVEDV), LV end-systolic volume (LVESV), LVEF, and LV GLS were measured according to the ASE recommendations (13). LV GLS was determined for an 18-segment LV model using 2D-STE from three apical views.
To assess LV diastolic function, the peak early diastolic mitral flow velocity (MV-E), peak late diastolic mitral flow velocity (MV-A), peak early diastolic velocity of the septal mitral annulus (MV-e′-sep), peak early diastolic velocity of the lateral mitral annulus (MV-e′-lat), and tricuspid regurgitation velocity (TR) were measured, and the peak early diastolic mitral flow velocity/late diastolic mitral flow velocity (MV-E/A), peak early diastolic mitral flow velocity/average of the peak early diastolic velocity of septal and lateral mitral annulus (MV-E/e′), and left atrial volume index (LAVI) were calculated.
Statistical analysis
The statistical analyses and graphing were performed using SPSS 26.0 (IBM Corporation, Armonk, NY, USA) and GraphPrism 9.0 (GraphPad, La Jolla, CA, USA). The categorical variables are expressed as the frequency (percentage), while the continuous variables are expressed as the mean ± standard deviation. Normality plots with tests were performed using the Shapiro-Wilk test, and the assumption of homogeneity of variance was verified using Levene’s test. The categorical variables were analyzed using the chi-square test or Fisher’s exact test as appropriate. Comparisons among ≥ three groups were assessed using a one-way analysis of variance (ANOVA) with the Tukey-Kramer post-hoc test when the assumption of homogeneity of variance was met; otherwise, Welch’s one-way ANOVA with the Games-Howell post-hoc test was used. Correlations between QRS duration and cardiac synchrony were determined by a Pearson’s correlation analysis. Simple and multiple linear regression analyses were performed to determine the variables associated with RV GLS or LV GLS. Variables with values of P<0.20 in the simple linear regression analyses were subjected to the multiple regression models using the enter method, and the associations are expressed as the regression coefficients and 95% confidence intervals (CIs). For all the analyses, two-sided values of P≤0.05 were considered statistically significant.
Results
Clinical characteristics
The clinical characteristics of all the subjects are summarized in Table 1. The mean age of the isolated CRBBB patients was higher than that of the healthy subjects (50.0±9.1 vs. 44.1±10.2 years, P=0.01) but did not differ significantly from that of the isolated CLBBB patients (50.0±9.1 vs. 50.9±8.3 years, P=0.87). Systolic blood pressure in the isolated CLBBB patients was higher than that in the isolated CRBBB and healthy subjects (130.4±7.7 mmHg for the isolated CLBBB patients vs. 126.5±6.9 mmHg for the isolated CRBBB patients vs. 125.5±8.3 mmHg for the healthy subjects; P=0.009).
Table 1
| Parameters | Healthy (n=42) | CLBBB (n=44) | CRBBB (n=44) | P value |
|---|---|---|---|---|
| Age (years) | 44.1±10.2 | 50.9±8.3* | 50.0±9.1* | 0.002 |
| Male | 16 (38.1) | 17 (38.6) | 23 (52.3) | 0.31 |
| BSA (m2) | 1.75±0.19 | 1.73±0.17 | 1.79±0.20 | 0.32 |
| BMI (kg/m2) | 24.71±4.97 | 25.66±4.53 | 25.16±3.38 | 0.60 |
| Smoking status | 6 (14.3) | 9 (20.5) | 8 (18.2) | 0.75 |
| HR (beat/min) | 67.1±4.6 | 68.8±5.4 | 66.4±5.1 | 0.08 |
| SBP (mmHg) | 125.5±8.3 | 130.4±7.7* | 126.5±6.9# | 0.009 |
| DBP (mmHg) | 80.6±3.1 | 79.8±6.3 | 78.4±7.4 | 0.22 |
| QRS duration (ms) | 105.3±5.2 | 156.2±11.0* | 153.7±15.1* | <0.001 |
| PR interval (ms) | 151.7±17.6 | 167.8±20.8* | 159.4±22.1 | 0.002 |
| QRS axis (°) | 38.5±29.6 | −2.8±28.5* | 48.5±44.7# | <0.001 |
| Synchrony | ||||
| LVDFT/RR (%) | 50.45±4.73 | 31.52±4.36* | 36.01±1.90*# | <0.001 |
| IVMD (ms) | 13.33±4.05 | 61.25±13.05* | 37.93±14.66*# | <0.001 |
| MD-LV (ms) | 29.72±7.96 | 71.88±12.96* | 61.25±13.61*# | <0.001 |
| MD-RV (ms) | 36.83±10.71 | 56.38±7.19* | 72.07±11.79*# | <0.001 |
| RV function | ||||
| RV-base (mm) | 31.05±4.01 | 32.88±3.12 | 41.07±5.30*# | <0.001 |
| RV-mid (mm) | 21.53±3.07 | 24.85±2.73 | 29.84±4.74*# | <0.001 |
| RVLD (mm) | 51.49±2.72 | 55.26±5.23 | 59.40±6.18*# | <0.001 |
| RV-Tei-Index | 0.40±0.09 | 0.67±0.19* | 0.76±0.14*# | <0.001 |
| RV-FAC (%) | 54.72±5.33 | 47.54±4.60* | 39.07±5.18*# | <0.001 |
| TAPSE (mm) | 21.97±2.46 | 21.56±2.93 | 15.24±1.94*# | <0.001 |
| TV-s′ (cm/s) | 12.62±1.92 | 11.48±2.36* | 8.68±0.98*# | <0.001 |
| RV GLS (%) | −25.70±3.51 | −23.30±3.82* | −18.53±4.95*# | <0.001 |
| RV-E/A | 1.45±0.31 | 1.29±0.41 | 1.19±0.32* | 0.003 |
| TV-E/e′ | 5.42±1.34 | 6.89±1.26* | 9.48±1.36*# | <0.001 |
| TV-EDT (ms) | 148.14±30.87 | 189.32±20.75* | 194.57±22.03* | <0.001 |
| LV function | ||||
| LVEDD (mm) | 47.64±2.40 | 51.79±4.95* | 49.69±4.83* | <0.001 |
| LVEDV (mL) | 90.55±8.18 | 101.77±19.50* | 99.23±28.05 | 0.001 |
| LVESV (mL) | 32.70±5.34 | 40.51±9.93* | 37.70±14.54 | <0.001 |
| LVEF (%) | 65.24±3.11 | 59.97±4.16* | 61.16±2.27* | <0.001 |
| LV GLS (%) | −21.23±1.46 | −16.96±1.41* | −17.98±1.51*# | <0.001 |
| MV-e′-sep (cm/s) | 10.17±1.48 | 5.57±1.53* | 7.70±2.78*# | <0.001 |
| MV-e′-lat (cm/s) | 12.40±2.65 | 7.77±2.50* | 10.82±2.74*# | <0.001 |
| MV-E/A | 1.48±0.44 | 0.80±0.26* | 1.01±0.36*# | <0.001 |
| MV-E/e′ | 7.52±2.09 | 13.83±4.55* | 10.93±1.45*# | <0.001 |
| LAVI (mL/m2) | 25.80±3.39 | 31.53±4.90* | 29.54±4.65* | <0.001 |
| TR (m/s) | 0.56±0.35 | 1.33±0.74* | 1.51±0.39* | <0.001 |
Data are expressed as the mean ± SD or n (%). *, P<0.05 vs. healthy controls; #, P<0.05 vs. CLBBB. CLBBB, complete left bundle branch block; CRBBB, complete right bundle branch block; BSA, body surface area; BMI, body mass index; HR, heart rate; SBP, systolic blood pressure; DBP, diastolic blood pressure; QRS duration, time interval between the Q-wave onset and the S-wave end; PR interval, time interval between the P-wave onset and the QRS-wave onset; QRS axis, angle between the frontal plane QRS-vector and horizontal axis; LVDFT/RR, the ratio of left ventricular diastolic filling time to the time interval between two adjacent R waves; IVMD, interventricular mechanical delay time; MD-LV, mechanical dispersion of the left ventricle; MD-RV, mechanical dispersion of the right ventricle; RV-base, right ventricular basal diameter; RV-mid, right ventricular mid diameter; RVLD, right ventricular longitudinal dimension; RV-FAC, right ventricular fractional area change; TAPSE, tricuspid annular plane systolic excursion; TV-s', systolic velocity of septal tricuspid annulus; RV GLS, right ventricular global longitudinal strain (six-segment); RV-E/A, peak early diastolic tricuspid flow velocity/late diastolic tricuspid flow velocity; TV-E/e′, peak early diastolic tricuspid flow velocity/peak early diastolic velocity of lateral tricuspid annulus; TV-EDT, deceleration time of the peak early diastolic tricuspid flow velocity; LVEDD, left ventricular end-diastolic diameter; LVEDV, left ventricular end-diastolic volume; LVESV, left ventricular end-systolic volume; LVEF, left ventricular ejection fraction; LV GLS, left ventricular global longitudinal strain; MV-e′-sep, peak early diastolic velocity of septal mitral annulus; MV-e′-lat, peak early diastolic velocity of lateral mitral annulus; MV-E/A, peak early diastolic mitral flow velocity/late diastolic mitral flow velocity; MV-E/e′, peak early diastolic mitral flow velocity/average of the peak early diastolic velocity of septal and lateral mitral annulus; LAVI, left atrium volume index; TR, tricuspid regurgitation velocity; SD, standard deviation.
The QRS duration of the isolated CRBBB patients was longer than that of the healthy subjects but did not differ from that of the isolated CLBBB patients (156.2±11.0 ms for the isolated CRBBB patients vs. 153.7±15.1 ms for the isolated CLBBB patients vs. 105.3±5.2 ms for the healthy subjects; P<0.001). The time interval between the P-wave onset and the QRS-wave onset (PR interval) of the isolated CRBBB patients did not differ significantly from that of the isolated CLBBB patients and healthy subjects, but the PR interval of the isolated CLBBB patients was longer than that of the healthy subjects (159.4±22.1 ms for the isolated CRBBB patients vs. 167.8±20.8 ms for the isolated CLBBB patients vs. 151.7±17.6 ms for the healthy subjects; P=0.002). The QRS axis in the isolated CLBBB patients was significantly more leftward than that in the isolated CRBBB and healthy subjects (48.5°±44.7° for the isolated CRBBB patients vs. −2.8°±28.5° for the isolated CLBBB patients vs. 38.5°±29.6° the for healthy subjects; P<0.001). There were no significant intergroup differences in terms of sex, body surface area, body mass index, smoking status, heart rate, or diastolic blood pressure.
Cardiac synchrony
LVDFT/RR was significantly decreased and IVMD, MD-LV, and MD-RV were significantly increased in the isolated CRBBB and CLBBB patients compared with the healthy subjects. IVMD and MD-LV were significantly decreased and LVDFT/RR and MD-RV were significantly increased in the isolated CRBBB patients compared to the CLBBB patients. The results suggested that atrioventricular, interventricular, right, and left intraventricular synchrony were significantly decreased in the isolated CRBBB and CLBBB patients compared to the healthy subjects. Compared to the isolated CLBBB patients, right intraventricular dyssynchrony was significantly decreased, but the degree of impairment of atrioventricular, interventricular, and left intraventricular dyssynchrony was lower in the isolated CRBBB patients (Table 1, Figures 2,3A-3D). Moreover, QRS duration was not significantly correlated with LVDFT/RR, IVMD, MD-LV, or MD-RV (r=−0.04, P=0.79; r=0.11, P=0.46; r=0.11, P=0.48; r=−0.06, P=0.71, respectively).
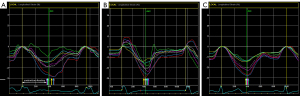

Comparison of RV function
RV-base, RV-mid, RVLD, RV GLS, TV-E/e′, TV-EDT, and RV-Tei-Index were significantly higher, and RV-FAC, TAPSE, and TV-s′ were significantly lower in the isolated CRBBB patients than the isolated the CLBBB patients and healthy subjects (Table 1); a graphical comparison of the RV GLS values among the groups is shown in Figure 3E. The RV systolic and diastolic function of the isolated CRBBB patients was significantly decreased compared to that of the isolated CLBBB patients and healthy subjects.
Comparison of LV function
The LV systolic and diastolic function parameters are shown in Table 1. The isolated CRBBB patients and isolated CLBBB patients had significantly decreased LV systolic and diastolic function compared to the healthy subjects as evidenced by the LV GLS, MV-E/A, and MV-E/e′ values. Compared with the isolated CLBBB patients, the isolated CRBBB patients had increased MV-E/A and decreased LV GLS and MV-E/e′ values. A graphical comparison of LV GLS values among groups is shown in Figure 3F. The LV function in the isolated CRBBB patients was more impaired than that in the healthy subjects, but the degree of impairment was less than that in the isolated CLBBB patients.
Factors associated with RV and LV systolic function in the isolated CRBBB patients
The results of the simple linear regression analyses showed that age, heart rate, MD-LV, and MD-RV were associated with RV GLS in the patients with isolated CRBBB. The results of the multiple linear regression analysis, which included four variables from the simple regression analyses, revealed that MD-RV was independently associated with RV GLS (coefficient, 0.13; 95% CI: 0.004–0.26; P=0.04), whereas the other factors showed no significant associations (Table 2).
Table 2
| Variables | Univariate regression | Multivariate regression† | |||
|---|---|---|---|---|---|
| Coefficient (95% CI) | P value | Coefficient (95% CI) | P value | ||
| Age (years) | −0.12 (−0.28, 0.51) | 0.17 | −0.08 (−0.23, 0.08) | 0.31 | |
| Male | 1.86 (−1.13, 4.85) | 0.22 | – | – | |
| BSA (m2) | 4.16 (−3.51, 11.83) | 0.28 | – | – | |
| HR (beat/min) | 0.24 (−0.05, 0.53) | 0.11 | 0.22 (−0.06, 0.49) | 0.12 | |
| QRS duration (ms) | −0.05 (−0.15, 0.05) | 0.31 | – | – | |
| PR interval (ms) | 0.01 (−0.07, 0.10) | 0.73 | – | – | |
| QRS axis (°) | −0.008 (−0.05, 0.03) | 0.71 | – | – | |
| SBP (mmHg) | 0.06 (−0.16, 0.28) | 0.61 | – | – | |
| DBP (mmHg) | −0.11 (−0.31, 0.10) | 0.30 | – | – | |
| LVDFT/RR (%) | 0.01 (−0.80, 0.82) | 0.98 | – | – | |
| IVMD (ms) | 0.03 (−0.08, 0.13) | 0.61 | – | – | |
| MD-LV (ms) | 0.09 (−0.01, 0.21) | 0.08 | 0.06 (−0.05, 0.17) | 0.29 | |
| MD-RV (ms) | 0.17 (0.05, 0.29) | 0.006 | 0.13 (0.004, 0.26) | 0.04 | |
†, the linear regressions of factors associated with RV GLS were performed using an enter method by clinical characteristics (including age, male, BSA, HR, QRS duration, SBP, and DBP) and synchrony parameters (including LVDFT/RR, IVMD, MD-LV, and MD-RV). Variables with P values <0.20 in the simple linear regression analyses were included in the multiple regression models. RV GLS, right ventricular global longitudinal strain (six-segment); CRBBB, complete right bundle branch block; CI, confidence interval; BSA, body surface area; HR, heart rate; QRS duration, time interval between the Q-wave onset and the S-wave end; PR interval, time interval between the P-wave onset and the QRS-wave onset; QRS axis, angle between the frontal plane QRS-vector and horizontal axis; SBP, systolic blood pressure; DBP, diastolic blood pressure; LVDFT/RR, the ratio of left ventricular diastolic filling time to the time interval between two adjacent R waves; IVMD, interventricular mechanical delay time; MD-LV, mechanical dispersion of the left ventricle; MD-RV, mechanical dispersion of the right ventricle.
In relation to the factors associated with LV GLS, the simple linear regression analysis results showed that body surface area, heart rate, PR interval, RV-base, RV-FAC, RV GLS, and LVDFT/RR were associated with LV GLS in the isolated CRBBB patients. Based on the simple linear regression analysis results, a multiple linear regression analysis showed that RV GLS (coefficient, 0.10; 95% CI: 0.01–0.20; P=0.03) and LVDFT/RR (coefficient, −0.30; 95% CI: −0.53 to −0.07; P=0.01) were independent factors of LV GLS (Table 3).
Table 3
| Variables | Univariate regression | Multivariate regression† | |||
|---|---|---|---|---|---|
| Coefficient (95% CI) | P value | Coefficient (95% CI) | P value | ||
| Age (years) | −0.002 (−0.05, 0.05) | 0.95 | – | – | |
| Male | 0.46 (−0.56, 1.47) | 0.37 | – | – | |
| BSA (m2) | 2.30 (0.03, 4.57) | 0.05 | 0.31 (−2.23, 2.84) | 0.82 | |
| HR (beat/min) | −0.07 (−0.16, 0.02) | 0.15 | −0.05 (−0.14, 0.04) | 0.28 | |
| QRS duration (ms) | −0.002 (−0.03, 0.03) | 0.88 | – | – | |
| PR interval (ms) | 0.02 (−0.003, 0.04) | 0.09 | 0.01 (−0.01, 0.03) | 0.34 | |
| QRS axis (°) | −0.002 (−0.01, 0.01) | 0.71 | – | – | |
| SBP (mmHg) | 0.04 (−0.03, 0.10) | 0.29 | – | – | |
| DBP (mmHg) | 0.02 (−0.04, 0.08) | 0.55 | – | – | |
| RV-base (mm) | 0.08 (−0.006, 0.16) | 0.07 | 0.07 (−0.03, 0.16) | 0.16 | |
| RV-mid (mm) | 0.02 (−0.09, 0.11) | 0.77 | – | – | |
| RVLD (mm) | 0.28 (−0.05, 0.10) | 0.47 | – | – | |
| RV-Tei-Index | 2.18 (−1.20, 5.56) | 0.20 | – | – | |
| RV-FAC (%) | −0.06 (−0.15, 0.03) | 0.15 | −0.007 (−0.10, 0.09) | 0.88 | |
| TAPSE (mm) | −0.07 (−0.31, 0.17) | 0.57 | – | – | |
| TV-s′ (cm/s) | 0.13 (−0.35, 0.61) | 0.58 | – | – | |
| RV GLS (%) | 0.10 (0.006, 0.19) | 0.04 | 0.10 (0.01, 0.20) | 0.03 | |
| RV-E/A | −0.28 (−1.77, 1.20) | 0.71 | – | – | |
| TV-E/e′ | 0.19 (−0.15, 0.53) | 0.26 | – | – | |
| TV-EDT (ms) | 0.003 (−0.02, 0.02) | 0.80 | – | – | |
| LVDFT/RR (%) | −0.30 (−0.53, −0.07) | 0.01 | −0.30 (−0.53, −0.07) | 0.01 | |
| IVMD (ms) | −0.001 (−0.03, 0.03) | 0.95 | – | – | |
| MD-LV (ms) | 0.02 (−0.02, 0.05) | 0.26 | – | – | |
| MD-RV (ms) | −0.003 (−0.04, 0.04) | 0.89 | – | – | |
†, the multiple linear regressions of the factors associated with LV GLS were performed using an enter method by clinical characteristics (including age, male, BSA, HR, QRS duration, SBP, and DBP), RV function parameters (including RV-base, RV-mid, RVLD, RV-Tei-Index, RV-FAC, TAPSE, TV-s′, RV GLS, RV-E/A, TV-E/e′, and TV-EDT) and synchrony parameters (including LVDFT/RR, IVMD, MD-LV, and MD-RV). Variables with P values <0.20 in the simple linear regression analyses were included in the multiple regression models. LV GLS, left ventricular global longitudinal strain; CRBBB, complete right bundle branch block; CI, confidence interval; BSA, body surface area; HR, heart rate; QRS duration, time interval between the Q-wave onset and the S-wave end; PR interval, time interval between the P-wave onset and the QRS-wave onset; QRS axis, angle between the frontal plane QRS-vector and horizontal axis; SBP, systolic blood pressure; DBP, diastolic blood pressure; RV-base, right ventricular basal diameter; RV-mid, right ventricular mid diameter; RVLD, right ventricular longitudinal dimension; RV-FAC, right ventricular fractional area change; TAPSE, tricuspid annular plane systolic excursion; TV-s', systolic velocity of septal tricuspid annulus; RV GLS, right ventricular global longitudinal strain (six-segment); RV-E/A, peak early diastolic tricuspid flow velocity/late diastolic tricuspid flow velocity; TV-E/e′, peak early diastolic tricuspid flow velocity/peak early diastolic velocity of lateral tricuspid annulus; TV-EDT, deceleration time of the peak early diastolic tricuspid flow velocity; LVDFT/RR, the ratio of left ventricular diastolic filling time to the time interval between two adjacent R waves; IVMD, interventricular mechanical delay time; MD-LV, mechanical dispersion of the left ventricle; MD-RV, mechanical dispersion of the right ventricle.
Discussion
The main findings of our study were as follows: (I) isolated CRBBB patients had impaired cardiac synchrony compared with the healthy subjects, and right intraventricular synchrony was especially decreased compared with the isolated CLBBB patients; (II) the RV systolic and diastolic function of the isolated CRBBB patients was decreased compared with that of the isolated CLBBB patients, and right intraventricular synchrony was independently associated with RV systolic dysfunction; (III) the LV systolic and diastolic function of the isolated CRBBB patients was decreased, but the degree of LV function impairment was less than that of the isolated CLBBB patients; and atrioventricular synchrony and RV systolic function were independently associated with the LV systolic function.
Isolated CRBBB: not completely benign
The right bundle branch consists of Purkinje fibers through the interventricular septum and provides rapid electric conduction to the RV free wall (22). Anatomically, the right bundle branch originates from the atrioventricular bundle and has a smaller and more discrete structure than the left bundle branch. Moreover, the blood of the proximal end of the right bundle branch is independently supplied by penetrating branches from the left anterior descending (LAD) coronary artery, but the left bundle branch receives a dual blood supply from the LAD coronary artery and the posterior descending branch. Therefore, the right bundle branch is more vulnerable to injury than the left bundle branch (23,24).
CRBBB is generally considered benign (9,10); however, recent studies have reported that CRBBB was related to poor clinical outcomes. Meyer et al. (25) showed that right bundle branch block was associated with high baseline cardiovascular risk in acute myocardial infarction patients, and CRBBB was an independent predictor of cardiovascular events in type 2 diabetes mellitus (26). In addition, a meta-analysis by Xiong et al. (27) revealed that right bundle branch block was related to an increased mortality risk in heart failure patients and the general population, which confirms that right bundle branch block portends a higher mortality risk, and thus deserves more attention and is worthy of investigation.
Impact of dyssynchrony on RV function in isolated CRBBB
When a block occurs along the right bundle branch, the electrical impulse activating the RV free wall originates from the left bundle branch through the myocardial tissue (28,29). The velocity of conduction between cardiomyocytes was significantly lower than that of the Purkinje fibers. When the RV lateral wall is excited, the interventricular septum is in an effective or relatively refractory stage, and the distance from the interventricular septum to the RV free wall is different, resulting in a more regional heterogeneous contraction of the right ventricle. Previous studies have shown that RV dyssynchrony measured by echocardiography was correlated with RV function in CRBBB patients with structural heart diseases (30), but no conclusions have been reached about the situation in isolated CRBBB patients.
In our study, we found that RV synchrony was significantly decreased in the patients with isolated CRBBB, and atrioventricular, interventricular and left intraventricular synchrony was also significantly decreased, which may result from the initial depolarization vector moving from the left to the right side of the interventricular septum, causing an activation delay in the LV distal segments and changes in the mechanical stretch order throughout the heart (31). The small difference in MD-LV between the isolated CLBBB and CRBBB patients was interesting. It may be that the right-sided septum below the block site of the bundle branch was electrically activated by cell-to-cell conduction instead of the specialized Purkinje fibers, which affected the synchrony of the interventricular septum significantly, resulting in left intraventricular mechanical dyssynchrony in the isolated CRBBB patients. In addition, the degree of reduction of right intraventricular dyssynchrony was greater, but the degrees of reduction of atrioventricular, interventricular, and left intraventricular dyssynchrony were less in the isolated CRBBB patients than the isolated CLBBB patients, which may be because the right bundle branch is mainly responsible for the electrical activation of the right ventricle and dominates a smaller area of myocardium than the left bundle branch.
RV function is a dependent factor with heart failure, clinical deterioration, and cardiovascular prognosis, and has received increased attention from clinicians recently (32-34). To accurately detect subclinical alterations in RV systolic function in the isolated CRBBB patients, we used RV GLS based on 2D-STE, which is a sensitive parameter recommended by the ASE guidelines (35). In our study, RV systolic function was significantly lower in the isolated CRBBB patients than the isolated CLBBB patients, while right intraventricular synchrony was independently associated with RV systolic function, but other clinical and synchrony parameters were not. The possible mechanism here is that the full filling and contraction of the right ventricle in the entire cardiac cycle cannot be guaranteed due to cardiac mechanical contraction dyssynchrony, and its efficiency during systole and diastole is decreased. In addition, RV mechanical contraction dyssynchrony may affect coronary perfusion coupled with changes in intraventricular hemodynamics, leading to uneven myocardial stretch, RV dilation, or remodeling.
LV function in isolated CRBBB
Surprisingly, our study results indicated that the deterioration of LV systolic function in the isolated CRBBB patients was independently associated with RV systolic function and atrioventricular synchrony. The reason may be that LV, RV, systemic circulation, and pulmonary circulation are a combination of volume, pressure, and electrical and mechanical activity. When CRBBB occurs, the presence of atrial ventricular dyssynchrony and RV systolic dysfunction leads to increased right atrial pressure and the delayed opening of the pulmonary valve, affecting atrial filling and emptying and thus changing LV systolic function. In addition, the blood supply to the right bundle branch comes mostly from the branch of the LAD coronary artery, which also supplies other major areas of the left ventricle, which might contribute to LV systolic dysfunction. Meanwhile, the isolated CLBBB patients also had decreased RV function, which might be due to the dual blood supply from the LAD coronary artery and posterior descending branch; however, the isolated CLBBB patients did not experience the same degree of impaired RV function because the LAD coronary artery provides the main blood supply to the left bundle branch (36).
Relationship of QRS duration with mechanical dyssynchrony
Our findings also showed that QRS duration was not correlated with cardiac synchrony; thus, it was an inadequate indicator of ventricular systolic dysfunction in patients with isolated CRBBB. Zaidi et al. demonstrated that QRS duration did not correspond to RV function in patients with hypoplastic left heart syndrome, while Uyguanco et al. showed that the prolongation of QRS duration is not a marker of significant LV systolic dysfunction in CRBBB patients with other structural heart diseases (29,37). Mechanical dyssynchrony measured by echocardiography is more sensitive and accurate than QRS duration on body surface ECG for assessing the underlying ventricular systolic dysfunction.
Limitations
The present study had several limitations. First, our study had a relatively small number of isolated CRBBB patients, which is likely a result of the relatively low prevalence of isolated CRBBB. We excluded patients with known causes of CRBBB to limit the effects of structural heart disease on systolic and diastolic function. Second, data on the effects of synchrony on long-term outcomes in patients with isolated CRBBB were lacking. However, there were few adverse cardiovascular events during the short-term follow-up period because CRBBB damage in patients is a long-term process. Third, the possibility of false-positive results were not absolutely excluded. MD-RV and MD-LV may increase in cases of regional dysfunction, which is unrelated to conduction delays. To minimize this possibility, we strictly excluded patients with any structural heart disease, any heart disease with possible regional dysfunction including ischemic heart disease, any history of coronary artery disease, or positive results on an exercise stress test. In addition, LVDFT/RR lacks specificity for atrioventricular dyssynchrony because it can be influenced by increased afterload when the difference of systolic blood pressure is significant; however, we did exclude patients with hypertension. Fourth, given that CRBBB is a common finding in patients with a concave-shaped chest wall and/or pectus excavatum (38) and that these individuals may exhibit intraventricular dyssynchrony and impaired biventricular myocardial strain parameters without any intrinsic myocardial dysfunction (39), further studies should be designed to evaluate the potential effects of chest wall conformation on cardiac synchrony and function in isolated CRBBB patients in comparison to isolated CLBBB patients.
Conclusions
The isolated CRBBB patients had impaired cardiac synchrony, biventricular systolic, and diastolic function compared with the healthy subjects. RV dyssynchrony and RV dysfunction in the isolated CRBBB patients were more decreased than in the isolated CLBBB patients, while the impairment degree of atrioventricular, interventricular, LV synchrony, and LV function in the isolated CRBBB patients was less than that in the isolated CLBBB patients. RV synchrony was independently associated with RV systolic function, while atrioventricular synchrony and RV systolic function were independently associated with LV systolic function. These findings suggest that we must perform more comprehensive echocardiography evaluations and monitor isolated CRBBB patients more closely.
Acknowledgments
We would like to thank Editage for the English language review.
Funding: This work was supported by the National Natural Science Foundation of China (grant No. U21A20387), and the National Natural Science Foundation of Liaoning Province (grant No. 2022-YGJC-63).
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://qims.amegroups.com/article/view/10.21037/qims-23-959/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://qims.amegroups.com/article/view/10.21037/qims-23-959/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013) and approved by the Ethics Committee of Medical Science Research of The First Hospital of China Medical University (No. 2019-93-2). Informed consent was obtained from all the participants.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Arham A, Bhardwaj R, Jain A, Dar I, Jain S, Warden B, Gharib W, Gharib W. Comorbidities of Chronic Complete Right Bundle Branch Block and Correlations With Coronary Angiographic Findings. Am J Med Sci 2016;351:97-100. [Crossref] [PubMed]
- Lévy S. Bundle branch blocks and/or hemiblocks complicating acute myocardial ischemia or infarction. J Interv Card Electrophysiol 2018;52:287-92.
- Fahy GJ, Pinski SL, Miller DP, McCabe N, Pye C, Walsh MJ, Robinson K. Natural history of isolated bundle branch block. Am J Cardiol 1996;77:1185-90. [Crossref] [PubMed]
- Akhtari S, Chuang ML, Salton CJ, Berg S, Kissinger KV, Goddu B, O'Donnell CJ, Manning WJ. Effect of isolated left bundle-branch block on biventricular volumes and ejection fraction: a cardiovascular magnetic resonance assessment. J Cardiovasc Magn Reson 2018;20:66. [Crossref] [PubMed]
- Valenti V, Zia MI, Shubayev L, Edelstein S, Supariwala A, Uretsky S, Fantozzi LM, Volpe M, Sciarretta S, Wolff SD. Cardiac magnetic resonance evaluation of the impact of interventricular and intraventricular dyssynchrony on cardiac ventricular systolic and diastolic function in patients with isolated left bundle branch block. Am J Cardiol 2012;110:1651-6. [Crossref] [PubMed]
- Wang Y, Li G, Ma C, Guan Z, Jin X, Li Y, Liu S, Yang J. Predictive Value of Septal Flash for Reduction of Left Ventricular Systolic Function as Reflected by Global Longitudinal Strain Using Echocardiography in Patients With Isolated Complete Left Bundle-Branch Block. Circ J 2018;82:2111-8. [Crossref] [PubMed]
- Alventosa-Zaidin M, Guix Font L, Benitez Camps M, Roca Saumell C, Pera G, Alzamora Sas MT, Forés Raurell R, Rebagliato Nadal O, Dalfó-Baqué A, Brugada Terradellas J. Right bundle branch block: Prevalence, incidence, and cardiovascular morbidity and mortality in the general population. Eur J Gen Pract 2019;25:109-15. [Crossref] [PubMed]
- Brooks N, Leech G, Leatham A. Complete right bundle-branch block: echophonocardiographic study of first heart sound and right ventricular contraction times. Br Heart J 1979;41:637-46. [Crossref] [PubMed]
- Niu HX, Hua W, Zhang S, Sun X, Wang FZ, Chen KP, Wang H, Chen X. Assessment of cardiac function and synchronicity in subjects with isolated bundle branch block using Doppler imaging. Chin Med J (Engl) 2006;119:795-800.
- Eriksson P, Wilhelmsen L, Rosengren A. Bundle-branch block in middle-aged men: risk of complications and death over 28 years. The Primary Prevention Study in Göteborg, Sweden. Eur Heart J 2005;26:2300-6. [Crossref] [PubMed]
- Sridhar AR, Padala SK. Isolated right bundle branch block in asymptomatic patients: not inconsequential as previously thought? Heart 2019;105:1136-7. [Crossref] [PubMed]
- Bussink BE, Holst AG, Jespersen L, Deckers JW, Jensen GB, Prescott E. Right bundle branch block: prevalence, risk factors, and outcome in the general population: results from the Copenhagen City Heart Study. Eur Heart J 2013;34:138-46. [Crossref] [PubMed]
- Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, Flachskampf FA, Foster E, Goldstein SA, Kuznetsova T, Lancellotti P, Muraru D, Picard MH, Rietzschel ER, Rudski L, Spencer KT, Tsang W, Voigt JU. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 2015;28:1-39.e14. [Crossref] [PubMed]
- Surawicz B, Childers R, Deal BJ, Gettes LS, Bailey JJ, Gorgels A, et al. AHA/ACCF/HRS recommendations for the standardization and interpretation of the electrocardiogram: part III: intraventricular conduction disturbances: a scientific statement from the American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology; the American College of Cardiology Foundation; and the Heart Rhythm Society. Endorsed by the International Society for Computerized Electrocardiology. J Am Coll Cardiol 2009;53:976-81. [Crossref] [PubMed]
- Strauss DG, Selvester RH, Wagner GS. Defining left bundle branch block in the era of cardiac resynchronization therapy. Am J Cardiol 2011;107:927-34. [Crossref] [PubMed]
- Moubarak G, Viart G, Anselme F. Acute correction of electromechanical dyssynchrony and response to cardiac resynchronization therapy. ESC Heart Fail 2020;7:1302-8. [Crossref] [PubMed]
- Cleland JG, Daubert JC, Erdmann E, Freemantle N, Gras D, Kappenberger L, Klein W, Tavazzi L. The CARE-HF study (CArdiac REsynchronisation in Heart Failure study): rationale, design and end-points. Eur J Heart Fail 2001;3:481-9. [Crossref] [PubMed]
- Ünlü S, Pagourelias E, Sezenöz B, Şahinarslan A, Uludağ OM, Gökalp G, Arınsoy T, Çengel A. Higher ultrafiltration rate is associated with right ventricular mechanical dispersion. Anatol J Cardiol 2019;21:206-13. [Crossref] [PubMed]
- Mele D, Luisi GA, Malagù M, Laterza A, Ferrari R, Bertini M. Echocardiographic evaluation of cardiac dyssynchrony: Does it still matter? Echocardiography 2018;35:707-15. [Crossref] [PubMed]
- Rudski LG, Lai WW, Afilalo J, Hua L, Handschumacher MD, Chandrasekaran K, Solomon SD, Louie EK, Schiller NB. Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J Am Soc Echocardiogr 2010;23:685-713; quiz 786-8. [Crossref] [PubMed]
- Muraru D, Onciul S, Peluso D, Soriani N, Cucchini U, Aruta P, Romeo G, Cavalli G, Iliceto S, Badano LP. Sex- and Method-Specific Reference Values for Right Ventricular Strain by 2-Dimensional Speckle-Tracking Echocardiography. Circ Cardiovasc Imaging 2016;9:e003866. [Crossref] [PubMed]
- Miller BE, Rajsheker S, López-Candales A. Right Bundle Branch Block and Electromechanical Coupling of the Right Ventricle: An Echocardiographic Study. Heart Views 2015;16:137-43. [Crossref] [PubMed]
- Li J, Li X, Dong S, Yang Y, Chu Y. Clinical characteristics and value in early reperfusion therapy for new onset right bundle branch block in patients with acute myocardial infarction. Exp Ther Med 2018;15:2620-6. [Crossref] [PubMed]
- Strauss DG, Loring Z, Selvester RH, Gerstenblith G, Tomaselli G, Weiss RG, Wagner GS, Wu KC. Right, but not left, bundle branch block is associated with large anteroseptal scar. J Am Coll Cardiol 2013;62:959-67. [Crossref] [PubMed]
- Meyer MR, Radovanovic D, Pedrazzini G, Rickli H, Roffi M, Rosemann T, Eberli FR, Kurz DJ. Differences in presentation and clinical outcomes between left or right bundle branch block and ST segment elevation in patients with acute myocardial infarction. Eur Heart J Acute Cardiovasc Care 2020;9:848-56. [Crossref] [PubMed]
- Ono K, Uchimoto S, Miyazaki M, Honda N, Mori K, Morioka T, Imai T, Shoji T, Emoto M. Complete Right Bundle Branch Block as a Predictor of Cardiovascular Events in Type 2 Diabetes. J Clin Med 2022;11:4618. [Crossref] [PubMed]
- Xiong Y, Wang L, Liu W, Hankey GJ, Xu B, Wang S. The Prognostic Significance of Right Bundle Branch Block: A Meta-analysis of Prospective Cohort Studies. Clin Cardiol 2015;38:604-13. [Crossref] [PubMed]
- Fantoni C, Kawabata M, Massaro R, Regoli F, Raffa S, Arora V, Salerno-Uriarte JA, Klein HU, Auricchio A. Right and left ventricular activation sequence in patients with heart failure and right bundle branch block: a detailed analysis using three-dimensional non-fluoroscopic electroanatomic mapping system. J Cardiovasc Electrophysiol 2005;16:112-9; discussion 120-1. [Crossref] [PubMed]
- Uyguanco ER, Mirandi A, Qureshi G, Lazar J, Chhabra A, Kassotis J. Prolongation of QRS duration and axis deviation in the right bundle branch block are not markers for left ventricular systolic dysfunction. Int J Angiol 2010;19:e83-5. [Crossref] [PubMed]
- Nakazawa N, Ishizu T, Seo Y, Kawamatsu N, Sato K, Yamamoto M, Machino-Ohtsuka T, Horigome H, Hiramatsu Y, Ieda M, Kawakami Y. The impact of right bundle branch block on right ventricular size and function assessed by three-dimensional speckle-tracking echocardiography. Heart Vessels 2020;35:576-85. [Crossref] [PubMed]
- D'Ascenzi F, Sanz-De La Garza M, Anselmi F, Nunno L, Arbelo E, Jordà P, Marzotti T, Aprile F, Piu P, Natali BM, Brugada J, Sitges M, Mondillo S. Electromechanical delay by speckle-tracking echocardiography: A novel tool to distinguish between Brugada syndrome and isolated right bundle branch block. Int J Cardiol 2020;320:161-7. [Crossref] [PubMed]
- Hamada-Harimura Y, Seo Y, Ishizu T, Nishi I, Machino-Ohtsuka T, Yamamoto M, Sugano A, Sato K, Sai S, Obara K, Yoshida I, Aonuma K. Incremental Prognostic Value of Right Ventricular Strain in Patients With Acute Decompensated Heart Failure. Circ Cardiovasc Imaging 2018;11:e007249. [Crossref] [PubMed]
- Tajima M, Nakayama A, Uewaki R, Mahara K, Isobe M, Nagayama M. Right ventricular dysfunction is associated with exercise intolerance and poor prognosis in ischemic heart disease. Heart Vessels 2019;34:385-92. [Crossref] [PubMed]
- Wu XP, Li YD, Wang YD, Zhang M, Zhu WW, Cai QZ, Jiang W, Sun LL, Ding XY, Ye XG, Qin YY, Lu XZ. Impaired Right Ventricular Mechanics at Rest and During Exercise Are Associated With Exercise Capacity in Patients With Hypertrophic Cardiomyopathy. J Am Heart Assoc 2019;8:e011269. [Crossref] [PubMed]
- Smolarek D, Gruchała M, Sobiczewski W. Echocardiographic evaluation of right ventricular systolic function: The traditional and innovative approach. Cardiol J 2017;24:563-72. [Crossref] [PubMed]
- Nikus K, Birnbaum Y, Fiol-Sala M, Rankinen J, de Luna AB. Conduction Disorders in the Setting of Acute STEMI. Curr Cardiol Rev 2021;17:41-9. [Crossref] [PubMed]
- Zaidi SJ, Penk J, Cui VW, Roberson DA. Right Ventricular Mechanical Dyssynchrony in Hypoplastic Left Heart Syndrome: Correlation with Systolic Function and QRS Duration. Pediatr Cardiol 2019;40:934-42. [Crossref] [PubMed]
- Tanner H, Bischof D, Roten L, Hoksch B, Seiler J, Schmid RA, Delacrétaz E. Electrocardiographic characteristics of patients with funnel chest before and after surgical correction using pectus bar: A new association with precordial J wave pattern. J Electrocardiol 2016;49:174-81. [Crossref] [PubMed]
- Sonaglioni A, Nicolosi GL, Trevisan R, Lombardo M, Grasso E, Gensini GF, Ambrosio G. The influence of pectus excavatum on cardiac kinetics and function in otherwise healthy individuals: A systematic review. Int J Cardiol 2023;381:135-44. [Crossref] [PubMed]


