
Rectal arteriovenous malformations with acute rectal hemorrhage: notable magnetic resonance imaging findings
Introduction
Intestinal arteriovenous malformation (AVM) is an abnormal connection between arteries and veins, mostly involving feeding arteries, malformed blood vessel groups, and draining veins. The clinical symptoms mostly consist of painless repeated intestinal bleeding, although severe anemia may occur in severe cases. The incidence of rectal AVM with rectal bleeding is low (1,2). Colonoscopy is reliable for the evaluation of rectal bleeding, but rectal AVM manifests as submucosal raised lesions or bowel wall congestion, edema, erosion, and hemorrhage, similar to submucosal lesions or ulcerative colitis. Colonoscopy has the advantage of allowing the operator to perform biopsy, but histopathological examination of the rectal mucosa in rectal AVM often only shows chronic inflammation resembling enteritis. Transrectal endoscopic ultrasonography is useful for detecting malformed vessels involved in rectal AVMs (3), but it is often difficult to perform in patients with persistent heavy bleeding. Digital subtraction angiography (DSA) is the gold standard for diagnosis, but DSA is not a routine examination, which means that diagnosing rectal AVM is challenging. Computerized tomography (CT) is a commonly used examination method, but a plain CT scan can only show the thickening of the rectal wall, which is consistent with the manifestation of enteritis, and does not contribute considerably to a definitive diagnosis. Enhanced CT scanning and CT angiography (CTA) can detect malformed blood vessels to clarify the cause. However, the application of iodine contrast agents involves risks and requires that patients be in a good physical condition. Magnetic resonance imaging (MRI) can show soft tissues in high resolution and has vascular flow void effects. The plain scan can clearly display the edematous bowel wall and malformed blood vessels in and around the bowel wall without the use of contrast agent. The aim of this paper is to characterize the MRI manifestations of rectal AVM via a case report and a review of the literature.
Case presentation
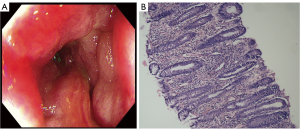
A 56-year-old male had a history of hemorrhoid surgery 20 years earlier. Hematochezia was noted 15 days prior to this admission. He was treated conservatively in another hospital for a week, but the response was poor, so he was referred to our hospital. Colonoscopy showed diffuse congestion, edema, erosion, and bleeding of the rectal mucosa (Figure 1A), and biopsy pathology showed chronic inflammatory infiltration in the intestinal mucosa (Figure 1B). During hospitalization, the patient experienced repeated massive rectal bleeding. Symptomatic and supportive treatment for hemostasis, blood transfusion, and anti-infective therapy were administered, but the response was also poor. Pelvic MRI was performed to determine whether there was a tumor or inflammatory lesion in or around the rectal wall. Diffuse thickening and edema of the rectal wall were observed (Figure 2A-2D). Diffuse, tortuous, and thickened empty blood vessels were observed around the rectum and in the rectal wall, suggesting the presence of rectal vascular malformation, particularly an AVM. We suspected that the patient’s repeated massive rectal acute bleeding was related to the AVM (Figure 2A-2D). Therefore, DSA was performed. DSA examination of the superior rectal artery revealed that in the tortuous malformed blood vessels, the feeding artery originated from the superior rectal artery, and the superior rectal vein was shown in advance and was the draining vein (Figure 3); therefore, the condition was treated with embolization of the superior rectal artery. The tortuous and dilated malformed vascular mass was not evident on contrast-enhanced imaging, and the remaining branches of the inferior mesenteric artery were well displayed. The patient’s condition improved significantly, and the rectal bleeding stopped. After 1 year of telephone follow-up, the patient had no blood in the stool or other discomfort. Unfortunately, no colonoscopy or imaging data are available.


All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
Acute rectal bleeding in rectal AVM resembles hemorrhoidal bleeding (4). Studies have shown that hemorrhoids may be associated with rectal AVM or other vascular malformations (5,6). It is worth noting that the patient we reported had hemorrhoidectomy 20 years prior. Unfortunately, there was no relevant imaging examination, and it is impossible to confirm whether the hemorrhoids were related to the patient’s rectal AVM. Rectal AVM is easily misdiagnosed as ulcerative enteritis (7) for several reasons. Firstly, its incidence is low. In our review of the relevant literature, a total of 29 articles on rectal vascular malformations combined with acute rectal bleeding were retrieved (Tables 1,2), including 12 articles on rectal AVM, with a total of 14 cases of rectal AVM being reported (Table 1) (8-17). Therefore, clinicians rarely consider this disease. Secondly, its clinical symptoms are nonspecific. Thirdly, the histopathological manifestations in the intestinal mucosa are similar to those of enteritis. Fourth, rectal mucosal colonoscopy findings are also similar to enteritis. Moreover, colonoscopy can only aid in the observation of the intestinal mucosa and not the situation inside or outside the intestinal wall.
Table 1
| Author | Year of publication | Diagnosis |
|---|---|---|
| Hirsch et al. (8) | 1976 | Anorectal arteriovenous malformation |
| Al-Humadi et al. (9) | 1979 | Arteriovenous malformation of the upper rectum |
| Yamanaka et al. (4) | 1981 | Arteriovenous malformation of the rectum |
| Ramírez Mayans et al. (10) | 1994 | Arteriovenous malformation of the rectum and sigmoid (3 cases) |
| Hayakawa et al. (11) | 1998 | Rectal arteriovenous malformation |
| McKevitt et al. (12) | 2002 | A polypoid rectal arteriovenous malformation |
| Pierce et al. (13) | 2010 | Perirectal arteriovenous malformation |
| Komekami et al. (6) | 2016 | Rectal arteriovenous malformation |
| Uchiyama et al. (14) | 2017 | Rectal arteriovenous malformation |
| Jubashi et al. (15) | 2021 | Rectal arteriovenous malformation |
| Fujinaga et al. (16) | 2021 | Rectal arteriovenous malformation |
| Krizzuk et al. (17) | 2022 | Rectal arteriovenous malformation |
Table 2
| Author | Year of publication | Diagnosis |
|---|---|---|
| Pumphrey et al. (18) | 1964 | Bleeding hemorrhoids caused by arteriovenous fistulas |
| Alm et al. (19) | 1980 | Rectal angiodysplasia |
| Tisnado et al. (20) | 1985 | Angiodysplasia of the rectum |
| Boukheloua et al. (21) | 1988 | Complex angiodysplasia of the recto-sigmoid |
| Beguiristain Gómez et al. (22) | 1989 | Colonic angiodysplasia (6 cecal and 1 rectal) |
| Vogt et al. (23) | 1990 | Extensive angiodysplasia of the colon and rectum |
| Vorobev et al. (24) | 1993 | Congenital angiodysplasias of the large intestine |
| Ayadi et al. (25) | 1994 | Rectal angiodysplasia |
| Jacquier et al. (26) | 2007 | Perirectal venous malformations. |
| Yap et al. (27) | 2013 | Rectal arterio-portal fistula |
| Bozkurt et al. (28) | 2014 | Rectal arteriovenous fistula |
| Ushigome et al. (29) | 2014 | Rectal arteriovenous fistula |
| Maddah et al. (30) | 2017 | Cavernous hemangioma of rectum |
| Ganesananthan et al. (31) | 2019 | Multiple venous malformations in the left colon and rectum |
| Wen et al. (32) | 2019 | Rectal arteriovenous fistula |
| Bhattacharjee et al. (33) | 2021 | Rectal venous malformation |
| Varela Recio et al. (34) | 2022 | Rectal arteriovenous fistula |
Diagnosing rectal AVM is challenging, and the choice of imaging examination method is critical. DSA is the gold standard for diagnosis, and enhanced CT and CTA examination can help aid in the clear diagnosis of rectal AVM, but the strict conditions for the application of contrast agents limit their application. Transrectal endoscopic ultrasonography is useful, but it is often difficult to perform in patients with persistent heavy bleeding. Under these conditions, MRI has obvious advantages in diagnosing rectal AVM owing to its high resolution of soft tissue and the presence of vascular flow voids. Bashir et al. reported that AVMs are high-flow vascular malformations, and distinguishing features include the presence of dilated tortuous vessels and flow voids on spin echo imaging, which manifest as signal voids on T1-weighted imaging and T2-weighted imaging (35). The same MRI findings were obtained in this case. Therefore, MRI is useful in diagnosing rectal AVM with acute rectal hemorrhage, especially in patients with contraindications to contrast agents. However, MRI also has disadvantages, namely, long imaging times, loud noise, and strict requirements for patient cooperation.
Conclusions
Given the typical MRI findings of rectal AVM, MRI has some advantages in showing the malformed vessels of rectal AVM.
Acknowledgments
We would like to thank the patient and the research assistants.
Funding: This work was supported by
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://qims.amegroups.com/article/view/10.21037/qims-23-609/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Hong J, Lee SY, Cha JG, Heo J. Unusual Presentation of Anal Pain and Tenesmus from Rectal Arteriovenous Malformation Successfully Treated with Ethanol Sclerotherapy. Case Rep Gastroenterol 2021;15:262-8. [Crossref] [PubMed]
- Hagihara PF, Chuang VP, Griffen WO. Arteriovenous malformations of the colon. Am J Surg 1977;133:681-7. [Crossref] [PubMed]
- Ishikawa S, Mukai S, Hirata Y, Kohata A, Kai A, Namba Y, Okimoto S, Fujisaki S, Fukuda S, Takahashi M, Fukuda T, Ohdan H. Rectal Arteriovenous Malformation Treated by Transcatheter Arterial Embolization. Case Rep Gastroenterol 2020;14:7-14. [Crossref] [PubMed]
- Yamanaka N, Okamoto E, Kuwata K, Toyosaka A, Ohashi S, Hida T, Okazora T, Kokui U, Shimoyama T, Satomi M. A case of arterio-venous malformation of the rectum: presenting with similar findings of hemorrhoidal bleeding (author's transl). Nihon Shokakibyo Gakkai Zasshi 1981;78:1293-7.
- Kapuller LL, Pirtakhiia RV, Rivkin VL. Importance of arteriovenous anastomoses and cavernous structures of the rectum in the pathogenesis of hemorrhoids. Arkh Patol 1970;32:52-6.
- Komekami Y, Konishi F, Makita K, Mijin T, Onogawa A, Chochi T, Lee C, Yoshida T, Maeda T, Mitsusada M, Hasegawa S. Rectal arterio-venous malformation (AVM) with bleeding of an internal hemorrhoid. Clin J Gastroenterol 2016;9:22-6. [Crossref] [PubMed]
- Maddah G, Abdollahi A, Rouhbakhshfar O, Taraz Jamshidi S, Hassanpour M. Arteriovenous malformations of the colon: A report of two cases and review of the literature. Caspian J Intern Med 2017;8:52-5.
- Hirsch SA, Boehnke M. Ano-rectal arteriovenous malformation; an unusual site of massive hemorrhage. Am J Proctol 1976;27:53-4.
- Al-Humadi AH, Domaleski AF, Alford JE. Arteriovenous malformation of the upper rectum in an unusual site: report of a case and review of the literature. Dis Colon Rectum 1979;22:189-94. [Crossref] [PubMed]
- Ramírez Mayans J, Gómez Suárez R, Mora Tiscarreño MA, Cervantes Bustamante R, Mata Rivera N, Cuevas Schatz CF, Miguel Vargas M, Méndez Nieto C. Arteriovenous malformations of the intestine in children. Study of 8 cases and review of the literature. Acta Gastroenterol Latinoam 1994;24:159-68.
- Hayakawa H, Kusagawa M, Takahashi H, Okamura K, Kosaka A, Mizumoto R, Katsura K. Arteriovenous malformation of the rectum: report of a case. Surg Today 1998;28:1182-7. [Crossref] [PubMed]
- McKevitt EC, Attwell AJ, Davis JE, Yoshida EM. Diminutive but dangerous: a case of a polypoid rectal arteriovenous malformation. Endoscopy 2002;34:429. [Crossref] [PubMed]
- Pierce J, Matthews J, Stanley P, Panossian A, Ford H, Anselmo D. Perirectal arteriovenous malformation treated by angioembolization and low anterior resection. J Pediatr Surg 2010;45:1542-5. [Crossref] [PubMed]
- Uchiyama H, Hattori R. Collateral artery from arteriovenous malformation of the rectum in a patient with peripheral artery disease. J Vasc Surg 2017;65:542-3. [Crossref] [PubMed]
- Jubashi A, Yamaguchi D, Nagatsuma G, Inoue S, Tanaka Y, Yoshioka W, Hino N, Morisaki T, Ario K, Fukui K, Ishimaru H, Tsunada S. Successful retrograde transvenous embolization under balloon occlusion for rectal arteriovenous malformation. Clin J Gastroenterol 2021;14:594-8. [Crossref] [PubMed]
- Fujinaga K, Nakahashi H, Haruki Y, Kato K. A Cure Case of Rectal Arteriovenous Malformation with a Large Volume of Melena Caused by Surgery for Rectal Cancer. Gan To Kagaku Ryoho 2021;48:2076-8.
- Krizzuk D, Cotesta M, Galiffa G, Peluso I, Falbo F, Biancucci A, Puscio S, Michelotto C, Pasecinic C, Montalto GM, Sammartino F. Polypoid arteriovenous malformation of the rectum: A case report. Front Surg 2022;9:924801. [Crossref] [PubMed]
- Pumphrey RE. Profound anemia caused by bleeding hemorrhoids of the arterial type suggesting arteriovenous fistulas. Dis Colon Rectum 1964;7:319-20. [Crossref] [PubMed]
- Alm P, Bauer H, Hugander A, Jönsson PE, Owman T. Angiodysplasia--a common cause of rectal bleeding. Lakartidningen 1980;77:1632-4.
- Tisnado J, Cho SR, Beachley MC, Margolius DA. Transcatheter embolization of angiodysplasia of the rectum. Report of a case. Acta Radiol Diagn (Stockh) 1985;26:677-80. [Crossref] [PubMed]
- Boukheloua B, Rekhroukh H, Kheloufi C, Bouhadef A, Zerhouni A, Hammad A. Complex angiodysplasia of the recto-sigmoid in children. Chirurgie 1988;114:252-8.
- Beguiristain Gómez A, Elbusto Cabello A, Rodríguez Andrés JA, Cormenzana Lizarribar E, Del Campo Senosiain L, Orcolaga Alba R. Angiodysplasia of the colon: a presentation of 7 cases. Rev Esp Enferm Apar Dig 1989;76:233-7.
- Vogt P, Raab R, Freise J, Pichlmayr R. Extensive angiodysplasia of the colon and rectum as a cause of recurrent lower intestinal hemorrhage. Chirurg 1990;61:545-7.
- Vorobev GI, Salamov KN, Kuzminov AM. Congenital angiodysplasias of the large intestine. Khirurgiia (Mosk) 1993;74-8.
- Ayadi A, Pousse H, Soua H, Baizig I, Sfar MT, Mougenot JF, Rambaud C, Martelli H, Schmitz J. A rare cause of rectal hemorrhage in children: rectal angiodysplasia. Arch Pediatr 1994;1:493-6.
- Jacquier A, Gorincour G, Vidal V, Petit P. Bowel venous malformation associated with an aneurysm of the portal vein. Pediatr Radiol 2007;37:714-6. [Crossref] [PubMed]
- Yap HY, Lee SY, Chung YF, Tay KH, Low AS, Thng CH, Madhavan K. Rectal arterio-portal fistula: an unusual cause of persistent bleeding per rectum following a proximal spleno-renal shunt. World J Gastroenterol 2013;19:4087-90. [Crossref] [PubMed]
- Bozkurt A, Sözen M, Kırbaş I, Bilgiç I, Kasapoğlu B, Nadir I. Acute lower gastrointestinal bleeding originating from an arteriovenous fistula of superior rectal artery. Int J Colorectal Dis 2014;29:1433. [Crossref] [PubMed]
- Ushigome H, Hayakawa T, Morimoto M, Kitagami H, Tanaka M. Rectal arteriovenous fistula resected laparoscopically after laparoscopic sigmoidectomy: a case report. Asian J Endosc Surg 2014;7:56-9. [Crossref] [PubMed]
- Maddah G, Abdollahi A, Rouhbakhshfar O, Taraz Jamshidi S, Hassanpour M. Arteriovenous malformations of the colon: A report of two cases and review of the literature. Caspian J Intern Med 2017;8:52-5.
- Ganesananthan S, Barlow J, Durai D, Hawthorne AB. Multiple venous malformations in the left colon and rectum: a long-standing case managed conservatively and an update of current literature. BMJ Case Rep 2019;12:e227700. [Crossref] [PubMed]
- Wen L, Wang B, Cui H. Hematochezia Associated With Rectal Arteriovenous Fistula. Am J Gastroenterol 2019;114:858. [Crossref] [PubMed]
- Bhattacharjee HK, Nariampalli Karthyarth M, Suhani S, Goyal A, Das NR, Sharma R, Parshad R. Laparoscopic total mesorectal excision for rectal venous malformation: A case report with a brief literature review. Asian J Endosc Surg 2021;14:85-9. [Crossref] [PubMed]
- Varela Recio J, Gómez-Sánchez T, Camacho Marente V, Roldán Ortiz S, Pacheco García JM. Selective embolization of the superior rectal artery as a treatment of massive rectal bleeding in a patient with arteriovenous fistula. Gastroenterol Hepatol 2022;45:129-30.
- Bashir U, Shah S, Jeph S, O'Keeffe M, Khosa F. Magnetic Resonance (MR) Imaging of Vascular Malformations. Pol J Radiol 2017;82:731-41. [Crossref] [PubMed]


