
Crohn’s disease with acute gastrointestinal bleeding caused by perianal fistula: a case description
Introduction
Gastrointestinal bleeding (GIB) is a rare complication of Crohn’s disease (CD) and has an incidence of less than 5% (1). The source of bleeding is more commonly a blood vessel being eroded by a deep ulcer. A case was reported in which the side effect of medicine might have resulted in thrombocytopenia, which is a risk factor for GIB (2). However, few cases have been reported on GIB caused by perianal fistula in CD. We here report a case of an uncommon etiology of GIB in CD, which can serve as reminder to physicians to not neglect the perianal managements in patients with perianal CD.
Case presentation
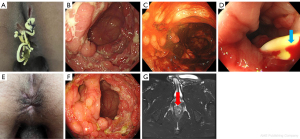
A 23-year-old male was hospitalized because of diarrhea lasting for 6 months. Before this, he had experienced no related symptoms or illnesses, and there was no indication of hereditary diseases. Twenty days before hospitalization, a complex fistula was found, and then seton placements (loose setons) were completed in another hospital due to the perianal fistula (Figure 1A). He was diagnosed with CD (A2, L3, B2, p) (Figure 1B) with normal vital signs and a hemoglobin level of 11.3 g/dL. Perianal magnetic resonance imaging indicated the presence of type 2 fistula according to the Parks classification system or grade 2 fistula according to the James classification. The inner openings were 10 mm from the anal margin, oriented at 4 and 6 o’clock respectively. Subsequently, a 5 mg/kg of infliximab was intravenously administered as induction therapy for perianal fistulizing CD. However, GIB appeared 5 days later. On the fifth day, acute GIB with more than 1,500 mL of hemorrhaging occurred in 1 hour. The patient was afebrile, with a blood pressure of 86/54 mmHg, a respiratory rate of 16/min, a heart rate of 118/min, and a hemoglobin level of 8.3 g/dL. An emergency colonoscopy revealed significant blood clots in the whole colon but not active bleeding. Hematic examination showed no coagulation disorders. Imagological examinations, including abdominal computed tomography, computed tomographic angiography, and abdominal angiography, revealed no vascular malformation, pseudoaneurysm, or diverticula. Fasting and somatostatin were applied, and blood and plasma transfusion were simultaneously used for rescue. Nevertheless, the levels of hemoglobin fluctuated in a range of 8.6–9.6 g/dL. Acute GIB occurred again after 10-day treatment, and active bleeding was discovered at the inner opening of the fistula but not in the sections of the colon that were indicated by the colonoscopy (Figure 1C,1D). Hot biopsy forceps were used to clamp the ruptured vessel so that the bleeding could be stopped. GIB did not occur in the following few days. Hence, the two occurrences of GIB were considered to be due to bleeding from the fistula. Following this, perianal hemostatic nursing was enhanced and involved softly rinsing the perianal skin, reducing friction stemming from clothes, and observing and recording the healing situation of the perianal skin, among other measures. Enteral nutrition was supplemented gradually. Finally, the patient was discharged without GIB, with mesalazine being the only treatment used in the following 2 months. At the end of April 2022, all loose setons were removed in the specialized hospital where the fistula was first treated since examinations showed that fistulizing drainage was sufficient, with no sign of infection. In May 2022, a physician restarted the treatment with infliximab (5 mg/kg with an 8-week interval). By July 2022, the external openings of perianal fistula had closed completely (Figure 1E), and colonoscopy showed few ulcers in the colon mucosa. (Figure 1F). The patient remained the disease remission without GIB until the last follow-up (September 21, 2022). All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
This case involved a rare etiology of acute GIB in CD. Initially, infliximab-related thrombocytopenia was once considered as the cause of GIB in this case due to the report of a similar case (2). However, age discrepancy, normal value of platelet count, and follow-up data did not support this possibility. Finally, the complex fistula treated by loose setons was regarded as the culprit lesion. Bleeding or a perianal hematoma after treatment has been reported in patients with complex fistula (3). In contrast to this case, the patient in the previous report (3) was treated with complex fistula via surgery, while our patient was treated with loose setons. The acute GIB in our case might have been related to the complex anatomy and adjacent structures of this type of fistula, where there are rectal arteriovenous and venous plexuses nearby. This patient experienced a complex perianal fistula in which the intrasphincteric-intersphincteric horseshoe fistula with 2 inner openings had several external openings (Figure 1G). He was treated with loose setons in another hospital before this hospitalization. Repeated mechanical irritation by the stool, infection by gut microbiota, and friction during the colonoscopy might have caused vascular injury of the perianal setons. Bleeding after vascular injury might have quickly caused a backflow into the gastrointestinal tract via one of the inner openings located in the anal canal and then led to acute lower GIB.
In conclusion, we treated a patient with CD and an acute GIB caused by a complex perianal fistula after seton therapy. It is important to pay attention to the protection of the perianal fistula, especially at the seton site of the fistula, during perianal invasive procedures. Moreover, should a similar situation arise in the future, we are resolved to promptly examine the perianal seton wound and complete perianal management to rule out this rare but relatively easy to manage cause of bleeding.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://qims.amegroups.com/article/view/10.21037/qims-23-311/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Podugu A, Tandon K, Castro FJ. Crohn's disease presenting as acute gastrointestinal hemorrhage. World J Gastroenterol 2016;22:4073-8. [Crossref] [PubMed]
- Boiten HJ, Amini S, Wolfhagen FHJ, Westerweel PE. Adalimumab-induced platelet antibodies resulting in severe thrombocytopenia. Br J Clin Pharmacol 2021;87:3619-21. [Crossref] [PubMed]
- Mushaya C, Bartlett L, Schulze B, Ho YH. Ligation of intersphincteric fistula tract compared with advancement flap for complex anorectal fistulas requiring initial seton drainage. Am J Surg 2012;204:283-9. [Crossref] [PubMed]


