Unexpected transesophageal echocardiography tee finding: mediastinal lipomatosis fakes an aortic intramural haematoma
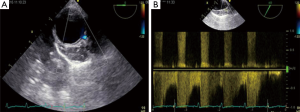
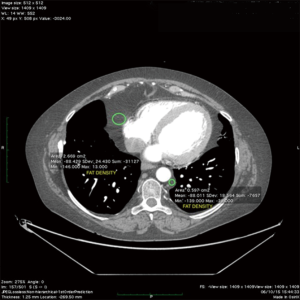
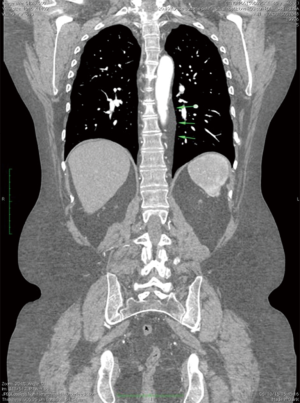
Mediastinal lipomatosis (ML) is a benign condition characterized by accumulation of fatty tissue. This condition is usually related to spontaneous or iatrogenic corticosteroid-induced Cushing syndrome or to obesity (1). Although it is an asymptomatic disorder, it can rarely result in compression of adjacent organs with thoracic pain, dyspnea, cough, dysphonia, and dysphagia. In this report we describe a case of fatty infiltration around descending aortic wall in a patient with autoimmune disorders, dilated cardiomyopathy and mitral insufficiency, simulating an intramural hematoma (IMH). A 49-year-old obese woman patient presented to our Heart Failure Outpatient Clinic for evaluation of progressive shortness of breath and sharp intermittent chest pain episodes. She was affected by dilated cardiomyopathy, systemic lupus erythematosus, rheumatoid arthritis on treatment with glucocorticoids, hyperlipidemia on treatment with statins and moderate renal dysfunction. On physical examination, her heart rate was 60 beats/min and regular, blood pressure was 130/70 mmHg bilaterally, carotid and peripheral pulses were normal bilaterally. A grade III/IV systolic murmur was heard at cardiac apex. Lung auscultation did not reveal any dry inspiratory crackles, as well as expiratory squeaks. On examination of extremities, neither digital clubbing or cyanosis or peripheral edema were noted. Trans-thoracic echocardiography showed mild left ventricular dilatation [left ventricular diastolic diameter (LVDD) 6 cm; LVDD/Body Surface Area (BSA) 3.3 cm/m2] with moderate reduction of global systolic function (ejection fraction 40%) and severe-moderate mitral regurgitation [effective regurgitant orifice area (EROA) was 4 cm2 in site of an eccentric jet directed toward the side wall of the left atrium) without any pericardial or pleural effusions. We decided to perform trans-esophageal echocardiogram (TEE) to screen the patient for percutaneous mitral valve repair (MVR) using the MitraClip system. Multiplane TEE showed moderate functional mitral regurgitation (3+/4+) associated with an unexpected remarkable new detail not consistent with previous diagnosis of precedent acute aortic syndrome. Indeed, withdrawing the TEE probe to visualize the descending aorta in short-axis (SAX) (0°) and long-axis (90°) views from the coeliac trunk to the left subclavian artery, as we use to perform to complete the exam, we recognized an hypoechoic, well-defined, crescent-shaped thickening of anterior aortic wall (>10 mm), mimicking IMH (Figure 1A). The descending aorta was no- dilated (diameter 2×2.2 cm2) and TEE assessment did disclose neither intimal flap nor laminar flow. The aortic lumen’s shape was preserved and the luminal wall was curvilinear and smooth. Color Doppler analysis detected a signal of demodulated systolic flow inside the crescent-shaped thickening of aortic wall, as intercostal vessels or aortic vasa-vasorum (Figure 1B). Therefore, in order to make an accurate differential diagnosis among aortic syndromes, a contrast-enhanced multidetector computed tomography (MDCT) was practiced, showing ML around descending aorta wall, without any sign of aortic dissection, and around the free wall of right ventricle.
Discussion
ML is a benign condition, related to obesity, iatrogenic o spontaneous Cushing syndrome. Rarely is a symptomatic condition, needing surgical decompression or reduction of the dosage of corticosteroids in the less severe forms (2). Few cases of ML are described in literature. Bulakci et al. reported a case of ML compressing the right ventricular outflow tract in a patient with Bechet disease, diagnosed with cardiac magnetic resonance imaging (MRI) (3). In addition, Sorhage et al. described an intrathoracic obstruction related to ML of the upper airway leading to symptoms of bronchial asthma (4). Finally Peek et al. reported a rare case of ML and severe aortic stenosis, mimicking an enormous cardiomegaly in which a plain chest X-ray showed bilateral widening of the mediastinal silhouette (5). In our case, TEE showed a crescent-shaped thickening of the anterior wall of descending aorta, mimicking an IMH. Of note, IMH can be difficult to distinguish from a thrombosed false lumen of classic aortic dissection because these can be both appear as a crescent-shape thickening of the aortic wall. The clinical scenario of our patient pushed us to require an urgent total body-MDCT to make the differential diagnosis and to exclude an aortic dissection. MDCT has greatly improved imaging of acute thoracic aortic (6-11) disease with excellent contrast and spatial resolution after administration of intravenous contrast medium. In our reported case MDCT allowed to distinguish the lumen of descending aorta (with perfect opacification in the arterial phase without signs of dissection) from the excess of adipose tissue surrounded the thoracic aorta. A region of interest (ROI) positioned in the context of component closely adjacent to the aorta, showing negative value, excluded the presence of aortic dissection supporting the evidence of ML along the descending aorta. Moreover redundant adipose tissue, with the same density of the tissue around the aorta, surrounded the right ventricle (Figures 2,3). We have scheduled a new MDCT scan for follow-up in next six months. To our knowledge, this is the first reported case describing ML around aortic wall simulating an IMH.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Gombar S, Mitra S, Thapa D, Gombar KK, Pathak R. Anesthetic considerations in steroid-induced mediastinal lipomatosis. Anesth Analg 2004;98:862-4. table of contents. [Crossref] [PubMed]
- Taillé C, Fartoukh M, Houël R, Kobeiter H, Rémy P, Lemaire F. Spontaneous hemomediastinum complicating steroid-induced mediastinal lipomatosis. Chest 2001;120:311-3. [Crossref] [PubMed]
- Bulakci M, Yahyayev A, Ucar A, Erer B, Erer B, Dursun M. Unusual cause of right ventricular outflow tract compression: mediastinal lipomatosis. J Thorac Imaging 2011;26:W134-6. [Crossref] [PubMed]
- Sorhage F, Stover DE, Mortazavi A. Unusual etiology of cough in a woman with asthma. Chest 1996;110:852-4. [Crossref] [PubMed]
- Peek DF, Heijmen RH, Ernst SM, Schepens MA. Extensive mediastinal lipomatosis in a patient with severe aortic valve stenosis. Eur J Cardiothorac Surg 2002;21:564-5. [Crossref] [PubMed]
- Valente T, Rossi G, Lassandro F, Rea G, Marino M, Urciuolo S, Tortora G, Muto M. MDCT distinguishing features of focal aortic projections (FAP) in acute clinical settings. Radiol Med 2015;120:50-72. [Crossref] [PubMed]
- Valente T, Rossi G, Lassandro F, Rea G, Marino M, Muto M, Molino A, Scaglione M. MDCT evaluation of acute aortic syndrome (AAS). Br J Radiol 2016;89:20150825. [Crossref] [PubMed]
- Valente T, Rossi G, Rea G, Pinto A, Romano L, Davies J, Scaglione M. Multidetector CT findings of complications of surgical and endovascular treatment of aortic aneurysms. Radiol Clin North Am 2014;52:961-89. [Crossref] [PubMed]
- Valente T, Rossi G, Lassandro F, Rea G, Marino M, Dialetto G, Muto R, Scaglione M. Unusual complications of endovascular repair of the thoracic aorta: MDCT findings. Radiol Med 2012;117:831-54. [Crossref] [PubMed]
- Rea G, Valente T, Iaselli F, Urraro F, Izzo A, Sica G, Muto M, Scaglione M, Muto M, Cappabianca S, Rotondo A. Multi-detector computed tomography in the evaluation of variants and anomalies of aortic arch and its branching pattern. Ital J Anat Embryol 2014;119:180-92. [PubMed]
- D'Alto M, Dimopoulos K, Budts W, Diller GP, Di Salvo G, Dellegrottaglie S, Festa P, Scognamiglio G, Rea G, Ait Ali L, Li W, Gatzoulis MA. Multimodality imaging in congenital heart disease-related pulmonary arterial hypertension. Heart 2016;102:910-8. [Crossref] [PubMed]


