
Subscapularis tendon tear detection using axial internal rotation MRI: semiquantitative and quantitative analysis
Introduction
Rotator cuff tendon tear is the leading cause of shoulder pain and long-term dysfunction (1). Over the last two decades, rotator cuff injury and arthroscopic-assisted surgery have become increasingly common (2,3). Subscapularis tendon injury is frequently missed at arthroscopy or surgery (4). Specific exploration of the subscapularis tendons under arthroscope increases diagnostic accuracy in subscapularis tendon pathology (5).
The subscapularis is one of the largest and strongest muscles in the rotator cuff (6). The muscle provides approximately 50 percent of rotator cuff force and plays a crucial role in dynamic and static shoulder stabilization (6-10). Subscapularis tendon tears are common. The reported prevalence of subscapularis tears among patients who underwent arthroscopy ranges from 12% to 50% (9,11-13). The most common site of subscapularis tendon tears is at the anterosuperior aspect and is often associated with long head biceps tendons pathology (4,14-20). Because the superior part of the subscapularis tendons adjoins the long head biceps tendons, it also supports long head bicep tendon stability (14,21). Delayed diagnosis or under detection of subscapularis tears may deteriorate shoulder function and provoke shoulder pain (4,22,23).
Magnetic resonance imaging (MRI) provides pathologic details and plays a crucial part in the preoperative diagnosis of subscapularis tendon tear. Axial and sagittal oblique views in fluid sensitive sequences are the most informative views in tendinous abnormality detection (7,10,14). Malavolta et al. (9) reported an overall sensitivity of 68% and overall specificity of 90% in the diagnosis of subscapularis tears. The sensitivity and specificity of full-thickness subscapularis tears are approximately 93% and 97%, respectively, while the sensitivity and specificity of partial tears are approximately 74% and 88%, respectively (9). Furukawa et al. (14) reported that radial-slice imaging magnetic resonance (MR) techniques improves the diagnostic value for subscapularis tears with a sensitivity of 94.7% and a specificity of 82.4%.
To improve the diagnostic sensitivity for partial- thickness subscapularis tears, we applied an internal rotation position using a fat-suppressed proton density (PD/FS) sequence scan on the axial plane in addition to the routine protocol. We hypothesize that the additional internal rotation position could increase the diagnosis accuracy of the partial subscapularis tendon tear on MRI. Therefore, we explored the advantages of this technique for the diagnosis of partial thickness subscapularis tendon tears and evaluated shoulder variations associated with subscapularis tendon tears and shoulder impingement. We present this article in accordance with the STARD reporting checklist (available at https://qims.amegroups.com/article/view/10.21037/qims-23-273/rc).
Methods
All MRIs of the shoulders between January 1st, 2018 and December 31st, 2019 in Siriraj hospital were retrospectively included in this study. The inclusion criteria were (I) MRI was performed within the 6 months preceding arthroscopy, (II) performed in a 3T MR machine, and (III) all axial PD/FS images, sagittal oblique fat-suppressed T2 weight image (T2W/FS) images and internal rotation axial PD/FS images were available. The exclusion criteria were (I) lack of demographic information or incomplete arthroscopic results; (II) complete tear of the subscapularis tendon in arthroscope; (III) presence of MR artifacts interfering image interpretation (e.g., metallic artifacts and motion artifacts); (IV) MRI with low image quality or improper shoulder position, and (V) MR images of patients with a history of bone or soft tissue tumors, bone fracture, infectious diseases, inflammatory arthritis, and previous surgery at shoulders. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Faculty of Medicine, Siriraj hospital, Mahidol University, Bangkok, Thailand, the Siriraj Institutional Review Board (No. SI039/2021) and individual consent for this retrospective analysis was waived.
A total of 1,011 MR images of the shoulders were performed between January 1st, 2018 and December 31st, 2019. Eighty-eight shoulder MRIs met the eligibility criteria. Eleven shoulder MRIs were excluded due to history of previous surgery at the shoulders, low image quality, or complete tear on arthroscopy. Another MRI was excluded due to the diagnosis of septic arthritis. As a result, 76 shoulder MRIs of 76 patients were enrolled. All patient underwent arthroscopy and physical examination by a sport medicine orthopedic surgeon (AK) and were grouped into no tear and partial groups. The clinical test data including belly press or lift off test, Jobe test, Neer test and Hawkin test were obtained.
Imaging acquisition
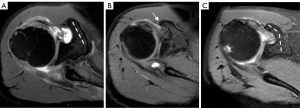
Three 3.0-T MR machines, including two Ingenia 3.0 T; Philips Healthcare, Best, Netherlands (installed in 2013 and 2014); and one MAGNETOM vida 3.0 T; Siemens, Erlangen, Germany (installed in 2019) were used. Phased array shoulder coils were also applied to the shoulders. For conventional MR images, patients were imaged supine with the humerus in the neutral position, the inner aspect of the arms adhering to the torsi, the thumbs pointing laterally, and the palms supinating. After conventional MR images were obtained, the internal rotation MR images were performed. The affected shoulders were passively flexed for 10–90 degree and the patients were asked to put the arms down and internally rotate the shoulders. The inner aspects of the arms were adhered to the torso with the thumbs pointed medially and palms pronating (Figure 1). The scanning parameters were listed as following; axial PD/FS and internal rotate PD/FS: repetition time (TR) =2,500 ms, echo time (TE) =30 ms, field of view (FOV) 140 mm, matrix =256×256; and sagittal T2W/FS: TR =3,870 ms, TE =75–80 ms, FOV 140 mm, matrix =256×256. The example of MR images is shown in Figure 2.

Imaging interpretation
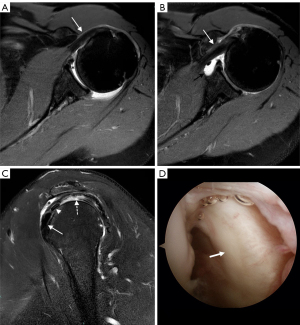
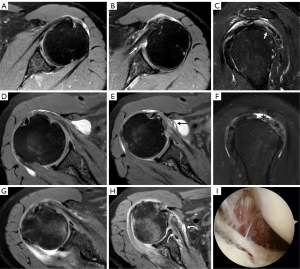
All shoulder MRIs were organized into three data sets. Set 1 was composed of axial PD/FS and sagittal T2W/FS images. Set 2 was axial PD/FS and internal rotation axial PD/FS images, and Set 3 was a combination of axial PD/FS, sagittal T2W/FS, and internal rotation axial PD/FS images. Two radiologists with eight and five years of experience in musculoskeletal radiology (PS and AP, respectively) independently reviewed the included MRIs. The three MRI sets were reviewed separately with a one-month gap between each MRI set. The reviewers were blinded to patient information (clinical histories, laboratory investigations and final diagnoses). Disagreements between the two reviewers were resolved by consensus. The morphology of MRIs for subscapularis and biceps tendons were classified as no tear, partial tear, and complete tear. Tendinosis of the subscapularis and biceps tendon were also recorded. Partial tears of the tendons were defined as evidence of fluid or near fluid signal intensity along the course of the tendon, particularly on the articular sides of the subscapularis tendons, without complete disruption of the tendon fibers (Figure 3). Complete tears of the tendons were defined as complete disruption of the tendinous course either with or without tendon retraction and were excluded from the study (Figure 4). Tendinosis was defined as increased signal intensity (less than fluid signal intensity) along the tendon without discontinuity or interruption of the tendon fibers (Figures 3,4).


Coracoid morphology was classified into three types (Figure 5). A flat coracoid type (type A) was defined as the axis of the coracoid process in the axial view is straight from the base to the tip. Type B is characterised by a prominent osteophyte at the end of the coracoid process. We defined hooked coracoid (type C) where the axis of coracoid process is laterally deviated a few centimeters at its base.
The coracohumeral distance (CHD) was measured as the narrowest point between the inner surface of the coracoid process or short head of the biceps tendon to the humeral head at level of mid glenohumoral joint (Figure 6A,6B). The coracoglenoid angle (CGA) was defined as an angle between a line from the anterior glenoid rim to the inner surface of the coracoid process and a line drawn perpendicularly to the glenoid surface at the level of the mid glenoid fossa (Figure 6C). The coracohumeral angle (CHA) was defined as an angle between a line drawn from the inner surface of the coracoid process to the lateral surface of humeral head and a line from the inner surface of the coracoid process to the medial surface of the humeral head (Figure 6D). All the measurements were made at the MRI image at the level that was able to visualize the widest diameter of the mid glenoid fossa. CHD difference was defined as the difference between the CHD measured in axial and internal rotation MR images. Coracohumeral ratio was defined as a ratio of the CHD measured in axial and internal rotation MR images.

Statistic analysis
Statistical analyses were performed using R version 3.4.3. Continuous data were described using a median and interquartile range, and categorical data were presented with a non-normal distribution and percentage. The Mann-Whiney U test was used to estimate the differences of continuous data between the two groups by arthroscopic diagnosis (tears and no tear of the subscapularis tendons). Chi-squared test or Fisher’s exact test was used for categorical data. A P value less than 0.05 was considered statistically significant.
Univariate and multivariable logistic regression was performed to determine the association of MRI variation parameters and the arthroscopic diagnosis. Multivariable models were performed to adjust for age, side, belly press or lift off test, Jobe test, CHD axial, CHD internal rotation, CHD different and CHD ratio. The association was presented as odds ratios (OR) with 95% confidence intervals (CI). The metrics for diagnostic performance were accuracy, sensitivity, specificity, positive predictive value, negative predictive value, and area under the receiver operating characteristics (AUROC). The cut-off value of each measurement parameter for diagnosing subscapularis tears was determined by Youden’s index. Agreements between two reviewers were tested with Kappa statistics. The Kappa index interpretation was considered as k <0 for no agreement; 0≤ k ≤0.20 for none to slight agreement; 0.20< k ≤0.40 for fair agreement; 0.40< k ≤0.60 for moderate agreement; 0.60< k ≤0.80 for substantial agreement; and 0.80< k ≤1 for almost perfect agreement for almost perfect agreement.
Results
Seventy-six shoulder MR images were retrospectively reviewed. Twenty-nine patients had a partial subscapularis tear under the arthroscope (38.2%), and 47 patients did not (61.8%) (Table 1). The median age of patients in the no tear and tear groups was 58 and 65 years, respectively (P=0.003). Fifty-six (73.6%) of patients underwent arthroscopy on the right shoulder with significant differences between groups (P=0.013). The Belly press or lift off test were found to be significantly positive more in the tear group (34.5%, P=0.011). The Jobe test also revealed significant differences between the tear and no tear groups (P=0.034). The Neer and Hawkins tests showed no significant differences between the groups (P=0.929 and P=0.531, respectively) (Table 1). Most patients in our study had a partial or complete supraspinatus tear (28.9% and 53.9%, respectively) without a significant difference between the groups (P=0.220). Most patients did not have a biceps tear (76.3%, P=0.056).
Table 1
| Parameters | Overall | Arthroscopic findings | P value | |
|---|---|---|---|---|
| Tear negative | Tear positive | |||
| Subjects (%) | 76 | 47 (61.8) | 29 (38.2) | |
| Age (years), median ± SD | 60.5±14 | 58.0±18 | 65.0±11 | 0.003 |
| Gender: female, n (%) | 41 (53.9) | 23 (48.9) | 18 (62.1) | 0.265 |
| Side: right, n (%) | 56 (73.6) | 30 (63.8) | 26 (89.7) | 0.013 |
| Clinical sign, n (%) | ||||
| Belly press or lift off test | 15 (19.7) | 5 (10.6) | 10 (34.5) | 0.011 |
| Jobe test | 49 (64.5) | 25 (55.3) | 23 (79.3) | 0.034 |
| Neer test | 37 (49.3) | 23 (48.9) | 14 (50) | 0.929 |
| Hawkin test | 34 (45.3) | 20 (42.6) | 14 (50) | 0.531 |
| Subscapularis tendinosis, n (%) | 57 (75.0) | 31 (66.0) | 26 (89.7) | 0.020 |
| Supraspinatus tendon, n (%) | 0.220 | |||
| Tear negative | 13 (17.1) | 12 (25.5) | 1 (3.4) | |
| Partial tear | 22 (28.9) | 14 (29.8) | 8 (27.6) | |
| Complete tear | 41 (53.9) | 21 (44.7) | 20 (69.0) | |
| Biceps tendon, n (%) | 0.056 | |||
| Tear negative | 58 (76.3) | 40 (85.1) | 18 (62.1) | |
| Partial tear | 13 (17.1) | 5 (10.6) | 8 (27.6) | |
| Complete tear | 5 (6.6) | 2 (4.3) | 3 (10.3) | |
| Biceps location: subluxation, n (%) | 1 (1.3) | 0 (0.0) | 1 (3.4) | 0.382 |
SD, standard deviation.
There was no statistically significant difference in coracoid morphology between the two groups (P=0.284) (Table 2). While type C coracoid was most common in the no-tear group (22/47 patients; 46.8%), type A coracoid was most common in the tear group (12/29 patients; 41.4%). The median of CHD axial were significantly wider in the tear group (6.20 vs. 6.94 mm; P=0.044) but the CHD during internal rotation were significantly narrowed in the tear group (6.62 vs. 5.78 mm; P=0.02). The measurement of the CGA, and the CHA were not significantly different between the two groups. The CHD difference and CHD ratio were significantly different (P<0.001) (Table 2).
Table 2
| Parameters | Overall | Arthroscopic findings | Odd ratio (95% CI) | P value | |
|---|---|---|---|---|---|
| Tear negative | Tear positive | ||||
| Subjects (%) | 76 | 47 (61.8) | 29 (38.2) | ||
| Coracoid morphology, n (%) | 0.284 | ||||
| Type A (R) | 24 (31.6) | 12 (25.5) | 12 (41.4) | 1 | |
| Type B | 21 (27.6) | 13 (27.7) | 8 (27.6) | 0.62 (0.19–2.02) | |
| Type C | 31 (40.8) | 22 (46.8) | 9 (31.0) | 0.41 (0.13–1.24) | |
| CHD axial (mm), median (IQR) | 6.48 (1.42) | 6.20 (1.16) | 6.94 (1.70) | 1.48 (1.03–2.11) | 0.044 |
| CHD internal rotation (mm), median (IQR) | 6.30 (1.53) | 6.62 (1.44) | 5.78 (1.57) | 0.68 (0.48–0.96) | 0.020 |
| CHA (degree), median (IQR) | 102.50 (10.75) | 101.00 (9.00) | 104.00 (14.00) | 1.03 (0.97–1.09) | 0.212 |
| CGA (degree), median (IQR) | 130.28 (5.84) | 130.57 (4.79) | 129.83 (7.31) | 0.98 (0.90–1.05) | 0.627 |
| CHD diff (mm), median (IQR) | 0.11 (1.59) | −0.40 (1.66) | 0.63 (1.33) | 2.58 (1.49–4.45) | <0.001 |
| CHD ratio, median (IQR) | 1.02 (0.27) | 0.94 (0.21) | 1.14 (0.20) | 1.34 (0.78–2.47) | <0.001 |
CI, confidence interval; MR, Magnetic resonance; IQR, interquartile range; CHD axial, coracohumeral distance measured in axial images; CHD internal rotation, coracohumeral distance measured in internal rotation images; CHA, coracohumeral angle; CGA, coracoglenoid angle; CHD diff, coracohumeral distance difference; CHD ratio, coracohumeral distance ratio; (R), the coracoid morphology type A is considering standard type and use as reference group in calculate odd ratio of other coracoid morphology types.
Diagnostic values of MRIs for subscapularis tendon tears
The diagnostic accuracy of MRIs for subscapularis tendon tears by the two reviewers using the MRI Sets 1, 2 and 3 was 61–66%, 67–68% and 75–76%, respectively (Table 3). With MRI Set 3, the diagnostic accuracy increased by approximately 10–14% when compared with MRI Set 1. The sensitivity of the diagnosis using the MRI Set 3 increased from 17–21% in Set 1 up to 79–83% in Set 3 (Table 3). The PPV using the MR image Set 3 slightly decreased from using the image data Set 1 and 2 in both reviewers. The negative predictive value (NPV) using the MRI Set 3 increased from the other two images data sets from both reviewers (Table 3).
Table 3
| Parameters | Reviewer 1 (95% CI) | Reviewer 2 (95% CI) | |||||
|---|---|---|---|---|---|---|---|
| MR Image Set 1 | MR Image Set 2 | MR Image Set 3 | MR Image Set 1 | MR Image Set 2 | MR Image Set 3 | ||
| Accuracy | 0.66 (0.54–0.76) | 0.68 (0.56–0.79) | 0.75 (0.63–0.84) | 0.61 (0.49–0.72) | 0.67 (0.55–0.77) | 0.76 (0.65–0.85) | |
| Sensitivity | 0.21 (0.80–0.40) | 0.31 (0.15–0.51) | 0.79 (0.60–0.95) | 0.17 (0.06–0.36) | 0.58 (0.39–0.76) | 0.83 (0.64–0.94) | |
| Specificity | 0.94 (0.82–0.98) | 0.91 (0.80–0.98) | 0.72 (0.57–0.84) | 0.87 (0.74–0.95) | 0.72 (0.57–0.84) | 0.72 (0.57–0.84) | |
| PPV | 0.67 (0.35–0.88) | 0.69 (0.43–0.87) | 0.64 (0.51–0.74) | 0.45 (0.22–0.71) | 0.57 (0.42–0.69) | 0.65 (0.53–0.75) | |
| NPV | 0.66 (0.61–0.70) | 0.68 (0.63–0.74) | 0.85 (0.73–0.92) | 0.63 (0.58–0.68) | 0.74 (0.64–0.82) | 0.87 (0.75–0.94) | |
MRI, magnetic resonance image; PD/FS, fat-suppressed proton density; T2W/FS, fat-suppressed T2 weighted; CI, confidence interval; PPV, positive predictive value; NPV, negative predictive value; MR, magnetic resonance imaging.
Observer agreement for MRI interpretation
The interobserver agreement in the interpretation of subscapularis tendon pathologies increased from a slight agreement in the MRI Sets 1 (0.08), to a substantial agreement in the MRI Set 2 and 3 (0.42 and 0.55, respectively) (Table 4). Additionally, the agreements in the diagnosis of subscapularis tendinosis increased from 0.47 to 0.55 using the MRI Set 1 and MRI Set 3, respectively.
Table 4
| MRI diagnosis | MR Image Set 1 | MR Image Set 2 | MR Image Set 3 | |||||
|---|---|---|---|---|---|---|---|---|
| Agreement | Kappa value | Agreement | Kappa value | Agreement | Kappa value | |||
| SSC tears | 78.95 | 0.08 | 75.00 | 0.42 | 77.63 | 0.55 | ||
| SSC tendinosis | 73.68 | 0.47 | 82.89 | 0.50 | 84.21 | 0.55 | ||
MRI, magnetic resonance image; SSC, subscapularis tendon; MR Image Set 1, axial fat-suppressed proton density weighted image (PD/FS) and sagittal oblique and sagittal fat-suppressed T2 weight image (T2W/FS) images; MR Image Set 2, axial PD/FS and internal rotation axial PD/FS; MR Image Set 3, axial PD/FS, internal rotation axial PD/FS and sagittal oblique T2WFS.
Association of quantitative parameters
Both the difference and the ratio of CHD between axial and internal rotation images were positively associated with the diagnosis of subscapularis tears with an OR of 2.58 (95% CI: 1.49–4.45) and 1.34 (95% CI: 0.78–2.47), respectively (Table 2). These parameters remained significant after multivariate analysis (P<0.001, both) (Table 5). Type C coracoid morphology was less likely to be found in the subscapularis tear group compared with the type A [OR =0.41 (95% CI: 0.13–1.24)] (Table 2). There were no statistically significant associations between subscapularis tears and other MRI measurement parameters. In addition, the Belly press or lift off test were also significant associated with subscapularis tear in multivariate analysis (Table 5).
Table 5
| Factor | Univariate analysis | Multivariate analysis | |||
|---|---|---|---|---|---|
| Odds ratio (95% CI) | P value | Odds ratio (95% CI) | P value | ||
| Age (years) | 1.064 (1.014–1.117) | 0.012 | – | ||
| Side: right | 0.204 (0.054–0.774) | 0.019 | – | ||
| Belly press or lift off test | 4.421 (1.328–14.716) | 0.015 | 4.795 (1.079–21.309) | 0.039 | |
| Jobe test | 3.096 (1.065–8.997) | 0.038 | – | ||
| CHD axial | 1.476 (1.033–2.108) | 0.032 | – | ||
| CHD internal rotation | 0.678 (0.478–0.962) | 0.030 | – | ||
| CHD diff | 2.576 (1.492–4.449) | 0.001 | 6.074 (2.380–15.500) | <0.001 | |
| CHD ratio | 1.397 (0.788–2.474) | 0.253 | 0.164 (0.055–0.487) | <0.001 | |
CHD, coracohumeral distance; CHD diff, coracohumeral distance difference; CHD ratio, coracohumeral distance ratio; CI, confidence interval.
The ratio of CHD on axial and internal rotation MRIs achieved the highest AUC at 0.85 (95% CI: 0.76–0.94), followed by the difference of CHD between the two different MRI views at 0.84 (95% CI: 0.76–0.93) (Figure 7). The AUC of the other MRI measurements were fairly low, particularly the measurements of coracohumeral and CGAs.

The cut-off value of each MRI measurement determined using Youden index is presented in Table 6. Given the cut-off value of the difference and ratio of CHD between axial and internal rotation positions at 0.04 mm and 1.01, the sensitivity was as high as 90% (0.73–0.98) and 90% (0.73–0.98), respectively. The specificity was also 72% (95% CI: 0.53–0.84) and 72% (95% CI: 0.53–0.84). With CGA more than 127.0 degrees, the specificity of diagnosing subscapularis tendon tears was as high as 85% (95% CI: 0.72–0.94) but low sensitivity 38% (95% CI: 0.21–0.58).
Table 6
| Parameters | Threshold | Sensitivity (95% CI) | Specificity (95% CI) | Accuracy (95% CI) | PPV (95% CI) | NPV (95% CI) |
|---|---|---|---|---|---|---|
| CHD axial | >6.81 mm | 0.58 (0.38–0.77) | 0.77 (0.62–0.88) | 0.70 (0.58–0.80) | 0.61 (0.46–0.74) | 0.75 (0.65–0.83) |
| CHD internal rotation | ≤6.82 mm | 0.76 (0.56–0.90) | 0.49 (0.34–0.64) | 0.59 (0.47–0.70) | 0.48 (0.39–0.56) | 0.77 (0.62–0.87) |
| CHA | >101 degree | 0.69 (0.49–0.84) | 0.47 (0.32–0.62) | 0.55 (0.43–0.67) | 0.44 (0.36–0.53) | 0.71 (0.57–0.82) |
| CGA | ≤127 degree | 0.38 (0.21–0.58) | 0.85 (0.72–0.94) | 0.67 (0.55–0.77) | 0.61 (0.41–0.78) | 0.69 (0.62–0.75) |
| CHD diff | >0.04 mm | 0.90 (0.73–0.98) | 0.72 (0.53–0.84) | 0.79 (0.68–0.88) | 0.67 (0.55–0.76) | 0.92 (0.79–0.98) |
| CHD ratio | >1.01 | 0.90 (0.73–0.98) | 0.72 (0.53–0.84) | 0.79 (0.68–0.88) | 0.67 (0.55–0.76) | 0.92 (0.79–0.98) |
MRI, magnetic resonance image; CI, confidence interval; CHD axial, coracohumeral distance measured in axial images; CHD internal rotation, coracohumeral distance measured in internal rotation images; CHA, coracohumeral angle; CGA, coracoglenoid angle; CHD diff, coracohumeral distance difference; CHD ratio, coracohumeral distance ratio; PPV, positive predictive value; NPV, negative predictive value.
Discussion
Semiquantitative evaluation of subscapularis tendons
The reported diagnostic performance of MRIs for subscapularis tendon tears has varied widely. In 2019, a meta-analysis conducted by Malavolta et al. (9) based on conventional MRI and MR arthrography using arthroscopy as the gold standard, revealed that the sensitivity and specificity of subscapularis tendon partial-thickness tears were 68% and 90%, respectively. The mean range of the sensitivity in the study were from 25% to 94% representing marked inconsistency of their data pool. Similarly, Furukawa et al. in 2014 (14), reported that a low-intermediate sensitivity (68.4%) but high specificity (100%), with 78.2% accuracy. The author suspicious difficulty in diagnosing subscapularis tendon pathologies to be due to oblique orientation of subscapularis tendon on axial plane. The partial volume effect could cause distortion of the tendinous courses (9,14). In our study, the diagnostic performance of conventional MRI using conventional sequences (MRI Set 1) had a low sensitivity (23–26%).
To our knowledge, our study is the first to use an internal rotation position on MRI to improve diagnostic performance for subscapularis tendon tears. Few previous studies mentioned that the internal rotation position may improve the detection of subscapularis pathologies, however, there is no consensus for the position yet (24,25). We found that using internal rotation combined with standard MR images (MRI Set 3) markedly improved the diagnostic accuracy to 75–76%, with moderate interobserver reliability (Kappa =0.55), compared to standard MR images alone (MRI Set 1, accuracy of 66–68%, and Kappa =0.08). The increased sensitivity of the internal rotation position we observed could have several explanations. First, the contraction of subscapularis muscles during internal rotation causes tension to the subscapularis tendons, generating a stress view of the tendon on internal rotation MR images. Second, the articular surfaces of the subscapularis tendons provide less contact area to the humoral heads while internal rotated, resulting in increased visualization of the tendinous articular surfaces. Third, when internally rotated the joint fluid accumulates in the anterior joint spaces outlining the articular surfaces of the subscapularis tendons (Figures 2B,3B), creating an arthrographic effect to the articular surface of subscapularis tendon. Finally, the subscapularis tendons glide beneath the coracoid processes and the short head biceps tendons when the shoulder is internally rotated, causing stress to the inner surfaces of subscapularis tendons. This might assist in evaluation of subcoracoid impingement. Example of MR images of cases with partial subscapularis tear were demonstrated in Figure 8.
We found no significant association between the type of coracoid morphology and subscapularis tendon tears (P=0.284). The coracoid type C was the most frequent type (40.8%), which is consistent with an anatomical study by Dugarte et al. (26) and Asal et al. (27). Both studies found hooked type coracoid process to be most common among elderly subjects (37.5-49%). Asal et al. (27) reported that type C is correlated with subscapularis tendon pathologies. This difference could be due to the younger age of subjects in the Asal study, while our subjects were mostly elderly persons.
Parametric measurements
The average CHDs in our study (mean CHD axial =6.48 mm) were lower than the CHD in earlier studies (24,28,29) (9.9–11.0 mm). This could be due the shorter statures and lower muscle mass in the Asian population, especially among the elderly, that leads to smaller bone-tendon structures compared to European and US populations (30,31).
Our study found the CHD in the tear group to be wider than in the no-tear group (6.94 vs. 6.20 mm, P=0.044) and mostly has subscapularis tendinosis. This result is consistent with other studies reporting that alteration of the subcoracoid spaces is associated with subcoracoid impingement (24,27,28,32-35). However, some of these studies reported smaller CHD in the impingement group (9.9–11.0 vs. 5.5–8.6 mm) (24,28). This may be due to the different age groups and definitions of impingement versus tendon tear used in different studies. Most reports use “subcoracoid impingement” and “subscapularis tendon tears” interchangeably, without a clear definition. Subcoracoid impingement typically presents as shoulder pain, which occurs due to narrowing of the space between the coracoid process and the humerus. Most subcoracoid impingement cases are diagnosed clinically without imaging studies. On the other hand, tearing of subscapularis tendons can be related to subcoracoid impingement or isolated to such condition.
In our study, the mean CHD in conventional MR of more than 6.81 mm was the best cut-off point to predict subscapularis tendon tears, with a sensitivity of 58%, a specificity of 77%, and an accuracy of 70%. The AUC value of the CHD was 0.66 (95% CI: 0.53–0.78) (Figure 7).
The effect of internal rotation to CHD might reflect subscapularis tendon quality. During internal rotation, the CHD becomes narrow in patients with tears, creating a greater difference and ratio between CHD in conventional images and the internal rotation position (mean CHD diff =0.63 mm; mean CHD ratio = 1.14; P value <0.001, both). The odd ratios were 2.58 (95% CI: 1.49–4.45) for CHD difference and 1.34 (95% CI: 0.78–2.47), for the CHD ratio. The AUC values were 0.84 (95% CI: 0.74–0.92) for CHD difference and 0.85 (95% CI: 0.75–0.92), for the CHD ratio (Figure 7). Our results were consistent with previous studies that reported that the CHD became narrowest during maximal internal rotation (25,33). Gerber et al. (36) established that the distance between the coracoid and the humeral head decreased when the shoulder was positioned in 90–100 degrees forward flexion with internal rotation. Therefore, the internal rotation position generates a pressure (provocation) view of the subscapularis tendons. The greater CHD difference might reflect a decrease in stiffness of the subscapularis tendons, representing worsened tendinous quality. In addition, we found a significant difference in number of tendinosis cases between the no-tear and tear groups (P=0.02). Therefore, we suspect that the overall quality of the tendinosis in the tear group was poorer. Friedman et al. (28) conducted cine MRI of the internal rotation position and reported that impingement resulted in decreased thickness of soft tissue beneath the subcoracoid space, which was not seen in asymptomatic subjects. Our results confirm that internal rotation enhances visualization of the subscapularis tendons and improves detection of subscapularis abnormalities even when the tendons are redundant or folding at the subcoracoid regions.
CGA and CHA have been described as parameters in the prediction of subcoracoid impingement (27,34,36). However, neither angle had a significant difference between the no-tear and tear groups in our study (P=0.627 for CGA, P=0.212 for CHA). Gerber et al. (36) studied subcoracoid spaces in 47 shoulders and found that there was a positive correlation between subcoracoid impingement and small CGA, particularly when a small coracoid overlap was present. Watson et al. (34) revealed that mean CGA measured in the axial view in subscapularis tears group was smaller than in the control group (CGA 37.02 degrees and CHA 40.56 degrees; P>0.05). Asal et al. (27) reported a significant decrease in the CGA value in patients with subscapularis tendon pathologies. We also found that the mean CGA value in patients with subscapularis tears was smaller than in the normal tendon group (129.83 vs. 130.57 degrees; P=0.627). CHA has been reported to be associated with subscapularis tendon pathologies (27). Consistent with our findings, Asal et al. (27) established that the CHA value significantly increased in patients with subscapularis tendon pathologies. However, the difference we observed was not statistically significant (P=0.212). This could be explained by the fact that CGA and CHA represent coracoid position in relation to glenoid and humerus. These relationships may be altered in the presence of impingement. Our subjects included those with shoulder pain who had an MRI performed and did not focus on subcoracoid impingement patients.
Our retrospective study has several limitations. First, the retrospective design of our study caused the population in our study to not focused on subscapularis impingement and the MR studies were done by two model of MR machines. We enrolled all patients who had shoulder pain, who suspicious of any rotator cuff pathologies and underwent arthroscopy. Therefore, their clinical could be worsen as compared to general population. Second, the arthroscopy is an operator-dependent examination and there may be considerable variability between surgeons in the interpretation of shoulder abnormalities, especially for the subscapularis tendon, however, the study currently serves as the best gold standard for the evaluation of internal derangement of the shoulder. Third, the surgeons in our institute, who performed arthroscopy were aware of the MRI reports and may have been influenced by these reports in their assessment of shoulder pathology. Forth, the subscapularis itself is a major internal rotator of the shoulder. Therefore, it may not be technically possible for the patient with subcoracoid impingement to actively and fully internally rotate the shoulder, and the range of motion and chronicity of the partial tear further contribute to the variability of internal rotation degree for each patient. This limitation can significantly impact the clinical use of this method. However, in our study, all patients were able to successfully achieve active or passive internal rotation during scanning. Fifth, the position used in our study was not maximally internal rotation but instead followed the elbow position. However, using such position revealed increased consistency in internal rotation degree and was more favorable when the patient had shoulder pain. Finally, the interobserver agreement result between the two radiologists was only 0.08-0.55. This reflects the high dependence of the diagnostic method on observer capabilities in the diagnostic performance of axial internal rotation MRI.
Conclusions
The internal rotation position during MRI of the shoulder can significantly improve the diagnostic accuracy for partial subscapularis tendon tears. The use of internal rotation PD/FS images in combination with standard axial PD/FS and sagittal T2W/FS images provides the highest sensitivity and accuracy for the detection of partial subscapularis tears. The measurement of CHD axial, CHD internal rotation, CHD difference, and CHD ratio can be useful parameters to indicate subscapularis tears. The findings of this study may contribute to improved preoperative planning and management, as well as reducing the risk of delayed diagnosis and treatment of subscapularis tears.
Acknowledgments
Special thanks to Sorawat Sangkaew (Department of social medicine, Hatyai hospital, Songkhla, Thailand) for statistic consultant and analysis.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STARD reporting checklist. Available at https://qims.amegroups.com/article/view/10.21037/qims-23-273/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://qims.amegroups.com/article/view/10.21037/qims-23-273/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Faculty of Medicine, Siriraj hospital, Mahidol University, Bangkok, Thailand, the Siriraj Institutional Review Board (No. SI039/2021) and individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Yamamoto A, Takagishi K, Osawa T, Yanagawa T, Nakajima D, Shitara H, Kobayashi T. Prevalence and risk factors of a rotator cuff tear in the general population. J Shoulder Elbow Surg 2010;19:116-20. [Crossref] [PubMed]
- Colvin AC, Egorova N, Harrison AK, Moskowitz A, Flatow EL. National trends in rotator cuff repair. J Bone Joint Surg Am 2012;94:227-33. [Crossref] [PubMed]
- Jo YH, Lee KH, Kim SJ, Kim J, Lee BG. National Trends in Surgery for Rotator Cuff Disease in Korea. J Korean Med Sci 2017;32:357-64. [Crossref] [PubMed]
- Pfirrmann CW, Zanetti M, Weishaupt D, Gerber C, Hodler J. Subscapularis tendon tears: detection and grading at MR arthrography. Radiology 1999;213:709-14. [Crossref] [PubMed]
- Adams CR, Brady PC, Koo SS, Narbona P, Arrigoni P, Karnes GJ, Burkhart SS. A systematic approach for diagnosing subscapularis tendon tears with preoperative magnetic resonance imaging scans. Arthroscopy 2012;28:1592-600. [Crossref] [PubMed]
- Lee J, Shukla DR, Sánchez-Sotelo J. Subscapularis tears: hidden and forgotten no more. JSES Open Access 2018;2:74-83.
- Saremi H, Yousefi S, Rastgari S, Rabiei MAS. Accuracy of magnetic resonance imaging for subscapularis tendon tear comparison with arthroscopy. Advances in Human Biology 2019;9:236.
- Keating JF, Waterworth P, Shaw-Dunn J, Crossan J. The relative strengths of the rotator cuff muscles. A cadaver study. J Bone Joint Surg Br 1993;75:137-40. [Crossref] [PubMed]
- Malavolta EA, Assunção JH, Gracitelli MEC, Yen TK, Bordalo-Rodrigues M, Ferreira Neto AA. Accuracy of magnetic resonance imaging (MRI) for subscapularis tear: a systematic review and meta-analysis of diagnostic studies. Arch Orthop Trauma Surg 2019;139:659-67. [Crossref] [PubMed]
- Alilet M, Behr J, Nueffer JP, Barbier-Brion B, Aubry S. Multi-modal imaging of the subscapularis muscle. Insights Imaging 2016;7:779-91. [Crossref] [PubMed]
- Waldt S, Bruegel M, Mueller D, Holzapfel K, Imhoff AB, Rummeny EJ, Woertler K. Rotator cuff tears: assessment with MR arthrography in 275 patients with arthroscopic correlation. Eur Radiol 2007;17:491-8. [Crossref] [PubMed]
- Lee JH, Yoon YC, Jee S, Kwon JW, Cha JG, Yoo JC. Comparison of three-dimensional isotropic and two-dimensional conventional indirect MR arthrography for the diagnosis of rotator cuff tears. Korean J Radiol 2014;15:771-80. [Crossref] [PubMed]
- Narasimhan R, Shamse K, Nash C, Dhingra D, Kennedy S. Prevalence of subscapularis tears and accuracy of shoulder ultrasound in pre-operative diagnosis. Int Orthop 2016;40:975-9. [Crossref] [PubMed]
- Furukawa R, Morihara T, Arai Y, Ito H, Kida Y, Sukenari T, Horii M, Ikoma K, Fujiwara H, Kubo T. Diagnostic accuracy of magnetic resonance imaging for subscapularis tendon tears using radial-slice magnetic resonance images. J Shoulder Elbow Surg 2014;23:e283-90. [Crossref] [PubMed]
- Sakurai G, Ozaki J, Tomita Y, Kondo T, Tamai S. Incomplete tears of the subscapularis tendon associated with tears of the supraspinatus tendon: cadaveric and clinical studies. J Shoulder Elbow Surg 1998;7:510-5. [Crossref] [PubMed]
- Schaeffeler C, Waldt S, Holzapfel K, Kirchhoff C, Jungmann PM, Wolf P, Stat D, Schröder M, Rummeny EJ, Imhoff AB, Woertler K. Lesions of the biceps pulley: diagnostic accuracy of MR arthrography of the shoulder and evaluation of previously described and new diagnostic signs. Radiology 2012;264:504-13. [Crossref] [PubMed]
- Tung GA, Yoo DC, Levine SM, Brody JM, Green A. Subscapularis tendon tear: primary and associated signs on MRI. J Comput Assist Tomogr 2001;25:417-24. [Crossref] [PubMed]
- Walch G, Nove-Josserand L, Levigne C, Renaud E. Tears of the supraspinatus tendon associated with "hidden" lesions of the rotator interval. J Shoulder Elbow Surg 1994;3:353-60. [Crossref] [PubMed]
- Warner JJ, Higgins L, Parsons IM 4th, Dowdy P. Diagnosis and treatment of anterosuperior rotator cuff tears. J Shoulder Elbow Surg 2001;10:37-46. [Crossref] [PubMed]
- Opsha O, Malik A, Baltazar R, Primakov D, Beltran S, Miller TT, Beltran J. MRI of the rotator cuff and internal derangement. Eur J Radiol 2008;68:36-56. [Crossref] [PubMed]
- Arai R, Sugaya H, Mochizuki T, Nimura A, Moriishi J, Akita K. Subscapularis tendon tear: an anatomic and clinical investigation. Arthroscopy 2008;24:997-1004. [Crossref] [PubMed]
- Lafosse L, Jost B, Reiland Y, Audebert S, Toussaint B, Gobezie R. Structural integrity and clinical outcomes after arthroscopic repair of isolated subscapularis tears. J Bone Joint Surg Am 2007;89:1184-93. [Crossref] [PubMed]
- Richards DP, Burkhart SS, Lo IK. Subscapularis tears: arthroscopic repair techniques. Orthop Clin North Am 2003;34:485-98. [Crossref] [PubMed]
- Giaroli EL, Major NM, Lemley DE, Lee J. Coracohumeral interval imaging in subcoracoid impingement syndrome on MRI. AJR Am J Roentgenol 2006;186:242-6. [Crossref] [PubMed]
- Brunkhorst JP, Giphart JE, LaPrade RF, Millett PJ. Coracohumeral Distances and Correlation to Arm Rotation: An In Vivo 3-Dimensional Biplane Fluoroscopy Study. Orthop J Sports Med 2013;1:2325967113496059. [Crossref] [PubMed]
- Dugarte AJ, Davis RJ, Lynch TS, Schickendantz MS, Farrow LD. Anatomic Study of Subcoracoid Morphology in 418 Shoulders: Potential Implications for Subcoracoid Impingement. Orthop J Sports Med 2017;5:2325967117731996. [Crossref] [PubMed]
- Asal N, Şahan MH. Radiological Variabilities in Subcoracoid Impingement: Coracoid Morphology, Coracohumeral Distance, Coracoglenoid Angle, and Coracohumeral Angle. Med Sci Monit 2018;24:8678-84. [Crossref] [PubMed]
- Friedman RJ, Bonutti PM, Genez B. Cine magnetic resonance imaging of the subcoracoid region. Orthopedics 1998;21:545-8.
- Lo IK, Parten PM, Burkhart SS. Combined subcoracoid and subacromial impingement in association with anterosuperior rotator cuff tears: An arthroscopic approach. Arthroscopy 2003;19:1068-78. [Crossref] [PubMed]
- Height and body-mass index trajectories of school-aged children and adolescents from 1985 to 2019 in 200 countries and territories: a pooled analysis of 2181 population-based studies with 65 million participants. Lancet 2020;396:1511-24. [Crossref] [PubMed]
- Seeman E. Growth in bone mass and size--are racial and gender differences in bone mineral density more apparent than real? J Clin Endocrinol Metab 1998;83:1414-9. [Crossref] [PubMed]
- Nair AV, Rao SN, Kumaran CK, Kochukunju BV. Clinico-Radiological Correlation of Subcoracoid Impingement with Reduced Coracohumeral Interval and its Relation to Subscapularis Tears in Indian Patients. J Clin Diagn Res 2016;10:RC17-20. [Crossref] [PubMed]
- Oh JH, Song BW, Choi JA, Lee GY, Kim SH, Kim DH. Measurement of Coracohumeral Distance in 3 Shoulder Positions Using Dynamic Ultrasonography: Correlation With Subscapularis Tear. Arthroscopy 2016;32:1502-8. [Crossref] [PubMed]
- Watson AC, Jamieson RP, Mattin AC, Page RS. Magnetic resonance imaging based coracoid morphology and its associations with subscapularis tears: a new index. Shoulder Elbow 2019;11:52-8. [Crossref] [PubMed]
- Hekimoğlu B, Aydın H, Kızılgöz V, Tatar IG, Ersan O. Quantitative measurement of humero-acromial, humero-coracoid, and coraco-clavicular intervals for the diagnosis of subacromial and subcoracoid impingement of shoulder joint. Clin Imaging 2013;37:201-10. [Crossref] [PubMed]
- Gerber C, Terrier F, Zehnder R, Ganz R. The subcoracoid space. An anatomic study. Clin Orthop Relat Res 1987;132-8.


