
Radiographic characteristics-based classification system for percutaneous endoscopic lumbar discectomy surgical approach selection in patients with L5–S1 disc herniation: a hierarchical clustering analysis
Introduction
Lumbar disc herniation (LDH), characterized by a displacement of nucleus pulposus beyond the physiological margins of the annulus fibrosus, is a prevalent disease of the spine (1). Due to changes in lifestyle, the incidence of LDH is increasing worldwide (2). Currently, surgical treatments of LDH are still warranted when the conservative treatment is recalcitrant (3). Percutaneous endoscopic lumbar discectomy (PELD), as a minimally invasive treatment method, is gradually becoming the first choice for LDH treatment because of its short operation time (OT), less blood loss, and quick recovery (4). PELD has gradually become the preferred treatment for LDH and lumbar spinal stenosis (5,6). To perform PELD, 2 surgical techniques were developed, percutaneous endoscopic transforaminal discectomy (PETD) and percutaneous endoscopic interlaminar discectomy (PEID) (4). PETD employs an “outside-in” approach to treating disc herniation and lumbar spinal stenosis that involves using a serial trephine and endoscope inserted into the spinal canal to address herniated disc matter, whereas PEID involves retracting the dural sac to address disc fragments, which may lead to dural laceration and further complications. (e.g., intervertebral infection, postoperative dysesthesia) (4,7). In cases when a puncture through the foramina (i.e., PETD) of the L5–S1 segment is challenging due to a high iliac crest, large transverse process of L5, large facet joint and narrow foramen, an interlaminar approach (i.e., PEID) may provide a better option (8-10). However, we have come across several cases of L5–S1 disc herniation in routine practice that show a relatively low iliac crest and a smaller transverse process of L5 which might be suitable for PETD. Regrettably, there has been no classification system for aiding the selection of surgical approaches and the determination of a surgical approach in patients with L5–S1 disc herniation is more commonly subjective, relying on the preference of spinal surgeons.
To date, several factors that might affect the choice of surgical approach have been determined including iliac height (IH), transverse process of L5, facet joint of S1, and intervertebral foramen size (10,11). Despite the current controversy, the height of the iliac crest has been considered an important determinant in deciding appropriate surgical approach among these factors; a higher iliac crest has been understood to indicate increased difficulty for surgeons to perform PETD. However, in clinical practice, difficulties in performing PETD have been encountered in patients with low iliac crest. This finding suggested that the ease of PETD could not be determined by the IH alone. Further, prior studies on this issue have mostly performed univariate analysis to explore the association between radiographic measures and surgical approaches (8,12). The utilization of pattern information from various radiographic metrics to assess lumbosacral anatomical morphology has not been adequately addressed or explored in previous studies. When the surgical approaches cannot be explained by the iliac crest alone, other radiographic metrics, such as the height of the intertransverse process and the width of the intervertebral foramen, might be potentially useful for aid the selection of surgical approaches (13). A more comprehensive characterization of the lumbosacral anatomical morphology might provide information for spinal surgeons to develop individualized surgical plans.
Therefore, in this study, we aimed to identify radiographic subtypes suitable for each PELD procedure in an unsupervised manner based on radiographic metrics measured from anteroposterior and lateral radiographs of the lumbar spine. The hierarchical clustering analyses were performed to identify radiographic subtypes, and several factors related to the ease of the surgery were compared between patients who underwent PEID and PETD in each subtype respectively. We present this article in accordance with the STROBE reporting checklist (available at https://qims.amegroups.com/article/view/10.21037/qims-23-277/rc).
Methods
Subjects
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Institutional Ethics Committee of Tianjin Hospital (No. 2023 medical ethical review 007). Written informed consent was provided by each participant prior to each procedure. For dataset 1: demographic and radiological data (i.e., anteroposterior and lateral radiographs of the lumbar spine) were retrospectively collected from 647 outpatients and inpatients in the Department of Radiology of Tianjin Hospital from January 2016 to October 2021. The detailed inclusion criteria for our current study were as follows: (I) intra-canal disc herniation; (II) radicular leg pain or back pain associated with disc herniation. The exclusion criteria were as follows: (I) history of surgery at L4–S1 segments; (II) obvious deformity or fracture of the lumbosacral vertebra; (III) unclear structure on radiograph; (IV) inconsistent height of iliac crest on each side; (V) under the age of 18 years. Therefore, total of 296 patients were included in our current study from dataset 1 (10).
Dataset 2: 111 patients with L5–S1 LDH who underwent PELD in the Minimally Invasive Spine Surgery Department of Tianjin Hospital from January 2016 to August 2022 were included retrospectively. Surgical procedures were performed by the same surgeon. The detailed inclusion criteria were as follows: (I) central, paracentral, and prolapsed disc herniation; (II) radicular leg pain or back pain associated with disc herniation; (III) failure of conservative treatments over 6 weeks. Exclusion criteria: (I) history of surgery at L4–S1 segments; (II) obvious deformity or fracture of the lumbosacral vertebra; (III) unclear structure on radiograph; (IV) inconsistent height of iliac crest on each side; (V) foraminal or extraforaminal disc herniation, highly migrated or calcified disc herniation; (VI) under the age of 18 (7,10). Figure 1 shows a flow diagram of the included patients.
Clinical assessment
The demographic data of the participants including gender and age were obtained through the radiographic system or medical record system for both dataset 1 and dataset 2. Surgery-related data included intraoperative blood loss (IBL), OT, and total operating room time (TORT) were retrospectively collected for dataset 2. OT was defined as the duration spanning from the preoperative fluoroscopy to the end of suture. The “ease” of surgery was defined based on quantitative variables measured during surgery, including IBL, OT, and TORT.
Preoperative visual analogue scale (VAS) scores (0–10) and the Oswestry Disability Index (ODI) scores (0–100%) were evaluated before surgery. Further, postoperative and discharge VAS scores (0–10) and the ODI scores (0–100%) were respectively collected 1 day after operation, as well as the data of discharge to assess clinical and functional outcomes (14).
Radiographic assessment
Radiographic measurements of metrics at the L5–S1 segment were performed in the validated software Vue PACS (Philips Healthcare, Amsterdam, Netherlands). All radiographic assessments were independently measured by 2 senior spine surgeons who were blind to the clinical information. For the validation of the assessments of 2 surgeons, the interobserver reliability was evaluated among the 2 “readers”. The intraclass correlation coefficient (ICC) two-way random model on agreement was used to assess the inter-observer reliability. ICC less than 0.40 was considered poor, 0.40–0.74 fair, 0.75–0.84 good, 0.85–0.89 very good, and equal or greater than 0.90 excellent (15). Further analyses were reperformed based on the average value for radiographic assessments obtained from 2 surgeons. The procedures for assessing each radiographic metric were as follows: coronal parameters: (I) intertransverse width (ITW): the distance from the outer side of the upper facet and the line linking the outer boundaries of the transverse processes and sacrum (16); (II) intertransverse height (ITH): the distance from the midpoint of the superior transverse process to the sacral wing (16); (III) interlaminar width (ILW): maximum lateral distance between lamina (17); (IV) interlaminar height (ILH): maximum vertical distance between lamina (17); (V) iliosacral angle (ISA): the angle formed between a tangent line touching the iliac crest and the line joining the highest point of the iliac crest and the superior-medial point of the S1 pedicle (10). Sagittal parameters: (VI) IH: the vertical distance between the highest point of the iliac crest and the midpoint of the S1 upper endplate (10); (VII) disc height (DH): the vertical distance between the lower endplate of the L5 vertebral body and the upper endplate of the sacrum (10); (VIII) IFH: the vertical distance from the lower margin of the L5 pedicle to the posterior upper endplate of S1 (10); (IX) intervertebral foramen width (IFW): the widest horizontal distance between the posterior vertebral line of L5 vertebral body and the superior facet of the S1 vertebra (10) (Figure S1). In dataset 1, considering that the images obtained from the sagittal view were of the right side of the participants, both coronal and sagittal radiographic assessments were conducted on the right side. In dataset 2, however, the sagittal assessments were conducted on the side which was performed PELD.
Data analysis
First, to explore the association among radiographic metrics, Spearman correlation coefficients were calculated in dataset 1. Subsequently, a dendrogram combined with Calinski-Harabasz index (CHI), Davies-Bouldin index (DBI), and Silhouette index (SI) were used to determine the optimal number of clusters. Hierarchical clustering was performed using radiographic parameters and demographic data based on homemade PYTHON script (https://github.com/changanyeyu/hierarchical-clustering) on 296 samples with Euclidean distance as distance metric in dataset 1. Afterwards, the average values of the radiographic metrics for each subtype were displayed in the radar map. Last, in dataset 2, the Euclidean distances were calculated for each patient between these patient’s radiographic measures and the mean of each subtype identified in dataset 1. Patients in dataset 2 were subsequently clustered based on which subtype they were close to. To explore the potential association between radiographic subtypes and the ease of PELD approaches, the IBL, OT, and TORT along with VAS and ODI were compared between patients identified as subtype 1 and subtype 2, following PETD or PEID procedures respectively, with age as covariates. Further, the surgeon’s preferred surgical approaches of each subtype were compared to verify the accuracy of our surgical decision. To further investigate the anatomic influence on surgical approach in real-word scenarios, anatomical parameters were compared between patients who underwent PEID and PETD.
Statistical analysis
D’Agostino-Pearson tests were carried out to check the normal distribution of the radiographic metrics and clinical measures, and QQ plots were also constructed to illustrate the normality of our data (Figures S2,S3). We performed 2-sample t-tests for continuous variables and employed the Chi-square test for categorical variables. Moreover, a parametric test was performed for parameters which passed the D’Agostino-Pearson tests, otherwise a nonparametric test was performed (i.e., Mann-Whitney test). All hypothesis tests were two-sided and the significance level was set at P<0.05.
Results
Demographic data
Demographic data of all participants are summarized in Table 1. The radiographic metrics of 296 patients were evaluated in dataset 1, including 141 males and 155 females with a mean age of 42.9±15.1 years. A total of 111 patients with L5–S1 LDH who underwent PELD were included in dataset 2. A total of 22 patients presented with central disc herniation; 26 patients exhibited left-sided paracentral disc herniation; 30 patients displayed right-sided paracentral disc herniation; and 33 patients displayed prolapsed disc herniation. The average extent of protrusion was 5 mm exhibiting a range from 2 to 10 mm. There were 55 males and 56 females with a mean age of 40.1±12.4 years.
Table 1
| Variables | Dataset 1 (n=296) | Dataset 2 (n=111) |
|---|---|---|
| Age (years) | 42.9±15.1 | 40.1±12.4 |
| Male sex | 141 (47.6) | 55 (49.5) |
Mean ± standard deviation is used to represent continuous variables while frequency and proportion (%) are used to represent categorical variables.
Inter-observer reliability
In dataset 1, the ICC values between the 2 observers’ measurements at ITW, ITH, ILW, ILH, ISA, IH, IFH, and IFW were 0.939 [95% confidence interval (CI): 0.924–0.951], 0.978 (95% CI: 0.972–0.982), 0.946 (95% CI: 0.933–0.957), 0.927 (95% CI: 0.909–0.942), 0.940 (95% CI: 0.926–0.952), 0.983 (95% CI: 0.979–0.986), 0.923 (95% CI: 0.904–0.938), and 0.906 (95% CI: 0.883–0.924), respectively, which was defined as excellent reliability. The value at DH was 0.887 (95% CI: 0.860–0.909) which was defined as very good reliability (Table S1). In dataset 2, the ICC values between the 2 observers’ measurements at ITW, ITH, ILW, ILH, ISA, IH, and IFW were 0.938 (95% CI: 0.911–0.957), 0.974 (95% CI: 0.962–0.982), 0.935 (95% CI: 0.907–0.955), 0.923 (95% CI: 0.889–0.946), 0.960 (95% CI: 0.942–0.972), 0.992 (95% CI: 0.988–0.994), and 0.921 (95% CI: 0.887–0.945), respectively, which was defined as excellent reliability. The value at DH and IFH were 0.894 (95% CI: 0.849–0.926) and 0.893 (95% CI: 0.848–0.925) which was defined as very good reliability (Table S1).
Correlation analyses
A significant positive correlation was observed between the following parameters: IH and ISA (R=0.75, P<0.001), IFH and ITH (R=0.53, P<0.001), IFW and ITH (R=0.40, P<0.001), and IFW and IFH (R=0.60, P<0.001). A significant negative correlation was observed between the following parameters: ISA and ITH (R=−0.42, P<0.001), IH and ITH (R=−0.46, P<0.001), IFH and IH (R=−0.42, P<0.001), IFW and ISA (R=−0.43, P<0.001), and IFW and IH (R=−0.50, P<0.001) (Figure 2).

Clustering analyses
By applying a dendrogram, the CHI, DBI, and SI, the optimal number of clusters was shown to be 2 in dataset 1 (Figure 3A,3B). Following hierarchical clustering, 2 subtypes were identified: subtype 1 with 205 samples and subtype 2 with a sample size of 91. The characteristics of the 2 subtypes were depicted in the radar map accompanied with the most representative images of each subtype (Figure 4). In subtype 1, the IH and the ITW were large with a small intervertebral foramen size and ITH. Subtype 2 exhibited a lesser IH and ITW along with a bigger intervertebral foramen size and ITH.


Comparation of clinical and functional outcomes along with surgical-related measures between different radiographic subtypes following PEID and PETD respectively
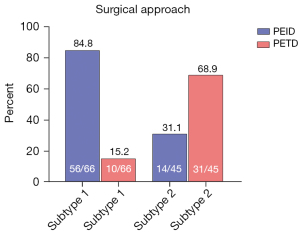
In dataset 2, for patients who underwent PEID, 56 patients were identified as subtype 1 and 14 patients were identified as subtype 2. For patients who underwent PETD, 10 patients were identified as subtype 1 and 31 patients were identified as subtype 2 (Table 2).
Table 2
| Variables | PEID | PETD | |||||
|---|---|---|---|---|---|---|---|
| Subtype 1 (n=56) | Subtype 2 (n=14) | P value | Subtype 1 (n=10) | Subtype 2 (n=31) | P value | ||
| ODI (%) | |||||||
| Pre-ODI | 60.0±9.5 | 62.3±12.2 | 0.447 | 62.0±13.3 | 57.9±9.2 | 0.280 | |
| Post-ODI | 13.6±3.1 | 13.7±4.0 | 0.919 | 12.9±3.5 | 12.7±3.4 | 0.873 | |
| Dis-ODI | 11.5±3.3 | 11.2±4.0 | 0.772 | 10.3±1.8 | 10.8±2.7 | 0.589 | |
| VAS-leg | |||||||
| Pre-VAS | 6.4±1.4 | 6.5±1.4 | 0.812 | 6.1±1.9 | 6.9±1.3 | 0.140 | |
| Post-VAS | 2.9±0.8 | 3.2±0.8 | 0.214 | 2.8±0.6 | 2.8±0.7 | >0.99 | |
| Dis-VAS | 2.0±0.9 | 2.0±0.8 | >0.99 | 1.7±0.7 | 1.9±0.7 | 0.437 | |
| VAS-back | |||||||
| Pre-VAS | 5.0±1.3 | 5.0±1.1 | >0.99 | 4.9±1.3 | 4.8±1.4 | 0.843 | |
| Post-VAS | 3.1±0.9 | 2.9±0.7 | 0.442 | 3.6±1.0 | 3.9±0.9 | 0.377 | |
| Dis-VAS | 2.1±0.8 | 2.0±0.6 | 0.663 | 2.7±1.1 | 2.7±0.9 | >0.99 | |
| OT (min) | 83.6±17.7 | 84.7±16.3 | 0.833 | 114.1±18.3 | 98.3±15.9 | 0.012 | |
| TORT (min) | 116.5±17.5 | 120.1±16.5 | 0.489 | 134.8±12.9 | 117.7±15.3 | 0.003 | |
| IBL (mL) | 18.8±8.6 | 15.4±6.0 | 0.168 | 34.5±18.0 | 20.2±11.7 | 0.006 | |
| Complications | 9 (16.1) | 2 (14.3) | >0.99 | 1 (10.0) | 4 (12.9) | >0.99 | |
| Never root injury | 0 | 0 | – | 0 | 1 (3.2) | >0.99 | |
| Recurrence rate | 3 (5.4) | 0 | >0.99 | 1 (10.0) | 1 (3.2) | 0.433 | |
| Dural tear | 2 (3.6) | 1 (7.1) | 0.494 | 0 | 0 | – | |
| Dysesthesia | 4 (7.1) | 1 (7.1) | >0.99 | 0 | 2 (6.5) | >0.99 | |
Mean ± standard deviation is used to represent continuous variables while frequency and proportion (%) are used to represent categorical variables. PEID, percutaneous endoscopic interlaminar discectomy; PETD, percutaneous endoscopic transforaminal discectomy; ODI, Oswestry Disability Index; Pre, preoperative; Post, postoperative; Dis, discharge; VAS, visual analogue scale; OT, operation time; TROT, total operating room time; IBL, intraoperative blood loss.
Patients with subtype 1 experienced a decrease in back and leg pain VAS scores from 5.0±1.3 to 3.1±0.9 (P<0.001) and 6.4±1.4 to 2.9±0.8 (P<0.001) after undergoing PEID; similar results were seen in patients who underwent PETD (4.9±1.3 to 3.6±1.0, P=0.022 and 6.1±1.9 to 2.8±0.6, P<0.001). Likewise, in subtype 2, VAS scores decreased from 5.0±1.1 to 2.9±0.7 (P<0.001) and 6.5±1.4 to 3.2±0.8 (P<0.001) in those who had the PEID procedure, and from 4.8±1.4 to 3.9±0.9 (P=0.004) and 6.9±1.3 to 2.8±0.7 (P<0.001) after PETD. The ODI score also improved significantly in both types of surgeries, with a reduction from 60.0±9.5 to 13.6±3.1 (P<0.001) in PEID patients and 62.0±13.3 to 12.9±3.5 (P<0.001) in PETD patients with subtype 1, from 62.3±12.2 to 13.7±4.0 (P<0.001) and 57.9±9.2 to 12.7±3.4 (P<0.001) in patients with subtype 2 (Table 2). These results indicate that both PEID and PETD provide equally effective treatments for herniated discs, with no significant differences between subtypes (Figure 5).

Relative to subtype 1, the patients identified as subtype 2 exhibited lesser IBL, shorter OT, and shorter TORT following PETD (t=2.92, P=0.006; t=2.65, P=0.012; t=3.17, P=0.003) whereas no significant differences in IBL, OT, and TORT were observed following PEID (t=1.43, P=0.168; t=0.22, P=0.833; t=0.69, P=0.489) (Figure 6).

A total of 11 complications occurred in patients who underwent PEID compared to 5 complications in those who underwent PETD, and the difference was not significant. One patient with subtype 2 experienced a neurological root injury in the PETD procedure, but successfully recuperated through conservative therapeutic measures. Among the patients with subtype 1 in the PEID, 3 experienced a recurrent LDH, whereas 1 patient with subtype 1 and 1 patient with subtype 2 experienced LDH recurrence in the PETD procedure. All these 5 cases accepted microdiscectomy revision surgeries. Furthermore, 2 patients with subtype 1 and 1 patient with subtype 2 encountered dural tears in the PEID procedure, all of whom recovered satisfactorily with conservative treatment. Dysesthesia was experienced by 4 patients with subtype 1 and 1 patient with subtype 2 in PEID, along with 2 patients with subtype 2 in PETD. Thankfully, all 7 patients showed significant improvement and were considered stable enough for discharge (Table 2).
After a comprehensive preoperative patient evaluation based on the surgeon’s own experience, about 68.9% (31/45) of patients with subtype 2 chose PETD whereas 84.8% (56/66) of patients with subtype 1 chose PEID (Figure 7).
Sub-analysis of anatomical factors between PEID and PETD
In dataset 2, 70 patients underwent PEID, whereas 41 patients underwent PETD. For coronal parameters, patients who underwent PETD demonstrated a lower ITW (P<0.0001), ISA (P<0.0001), and higher ITH (P<0.0001). For sagittal parameters, patients who underwent PETD exhibited a lower IH (P<0.0001), and a higher IFH (P<0.0001) and IFW (P<0.0001) (Figure 8).

Discussion
In our current study, 3 main findings were observed: (I) IH was negatively correlated with IFW, IFH, and ITH; ITH was positively correlated with IFW and IFH; (II) 2 lumbosacral radiographic subtypes were identified via hierarchical clustering analysis; and (III) relative to subtype 1 (i.e., a high iliac crest with a small size of intervertebral foramen) the patients identified as subtype 2 exhibited lesser IBL, and shorter OT and TORT following PETD whereas there were no significant differences IBL, OT, and TORT following PEID.
PETD and PEID are equally effective for the treatment of L5–S1 disc herniation
PELD which comprises translaminar (i.e., PEID) and transforaminal (i.e., PETD) approaches has a wide range of indications and were suitable for the treatment of intra-canal disc herniation, migrated disc herniation, and foraminal and extraforaminal disc herniation (4,9,18). Both techniques have been shown to be equally effective for the treatment of degenerative lumbar disease, such as LDH and partial lumbar spinal stenosis (19,20). Previous reports have also concluded that the VAS and ODI scores were not significantly different between the 2 PELD approaches, which were in line with our current findings, indicating that both techniques could significantly improve the quality of life and reduce pain in patients with L5–S1 disc herniation (9,11,21).
It is worth noting that the OT discussed in our manuscript differs from that mentioned in prior studies, as it contains the period of preoperative fluoroscopy to the end of suture rather than the interval between the skin incision and the completion of suturing (22,23). As a result, both of these procedures appear to require a greater amount of surgical time when compared to the traditional microdiscectomy procedure. Based on previous studies, the OT for performing PETD ranged from 61.9±9.6 to 97.5±15.5 minutes, whereas that for performing PEID ranged from 50.2±7 to 80.8±12.67 minutes (24). However, in our current study, the OT for subtype 1 and subtype 2 in PETD was 112.4±18.3 and 96.6±14.6 minutes, and in PEID, it was 83.5±17.5 and 85.2±16.8 minutes, respectively. The puncture process in patients with subtype 1 (i.e., high iliac crest with a small intervertebral foramen) poses numerous challenges, leading to a significantly prolonged duration for performing PETD. Besides, considering the process of fluoroscopy, surface location, sterilization, and draping, our OT remains within an acceptable range.
The iliac crest height is not the only determinant for the choice of PEID and PETD
PETD sometimes presents challenges due to anatomical factors when it comes to the segment of L5–S1 (4,10,21). The puncture needle passes through the superior border of the iliac crest and reaches the lesion through the tip of the superior articular process when performing PETD (25). As a result, the iliac crest, transverse process of L5, superior articular process of S1, and intervertebral foramen were shown to influence the ease of PETD. Among all these factors, the height of the iliac crest has been shown to be the most important factor that played a decisive role as the starting point for puncture. A higher iliac crest indicated more difficulties for spinal surgeons to penetrate through the intervertebral foramen and perform PETD. However, until now, the definition of a high iliac crest has remained controversial. Choi et al. defined the height of the iliac crest as the highest point of the iliac crest above the midpoint of L5 pedicle on the lateral radiograph, thus additional foraminoplasty was required for enlarging the intervertebral foramen to set up the endoscope (10). According to Song et al., patients could benefit from other surgical approaches than the PETD when the highest point of the iliac crest located above the lower edge of the L4 pedicle on the lateral radiograph (8). Increasingly, studies have shown that the iliac crest height is not the only factor influencing the choice of surgical approaches. It has been shown that not only the iliac crest, but the entire iliac wing area affects the PELD approaches, as the obstruction of the iliac wing margin from front to back may also have a significant effect on the surgery of the L5–S1 segment (8). Moreover, in clinical practice, difficulties in performing PETD have still been encountered in patients with low iliac crest still. These findings suggested that the ease of PETD could not be reflected by the IH alone; several other factors including transverse process of L5, superior articular process of S1, and intervertebral foramen size also have potential influences. Our current results identified 2 anatomical subtypes via multivariate clustering analyses, thus these subtypes would be more subjective and comprehensive as they considered the morphology of the entire lumbosacral region. Further, the ease of the procedure (PEID and PETD) was significantly different between the 2 subtypes. These findings indicated that the iliac crest height is not the only determinant for the choice of PEID and PETD, whereas the morphology pattern of the lumbosacral region would be more useful for the determination of surgical approaches.
L5–S1 anatomic subtypes for aiding the choice for PEID and PETD
Taking into consideration the fact that PETD offers great benefits, such as the use of local anesthesia and no need for dural stretching, whereas PEID requires traction of the dural sac which may cause dural laceration and nerve damage in addition to other related complications (4,26), PETD has been preferred by spine surgeons when treating degenerative lumbar diseases (27,28). Nonetheless, treating the L5–S1 segment with PETD might be difficult in some cases due to numerous factors that can affect its ease of execution (29). How to decide and chose the surgical approach for PELD treatment of L5–S1 segment is still based on the subjective preferences of spinal surgeons (30). Nevertheless, past studies have only focused on the iliac crest height as a deciding factor in the choice of surgical approaches and only performed univariate analysis, ignoring the potential contribution of the pattern information consisting of various morphological features. Our current study conducted an unsupervised clustering analysis and objectively identified 2 subtypes that might aid surgeons for selecting appropriate approach when performing L5–S1 PELD. Compared with subtype 1, subtype 2 exhibited smaller IH, ISA, and ITW, and greater ITH, IFW, and IFH. Anatomically, it is easier to perform PETD in subtype 2 than subtype 1, subsequent analysis of surgical-related information also confirmed this assumption. A shorter OT and TORT, and less IBL were observed in subtype 2 than those in subtype 1 patients following PETD. Similar to previous findings observed by univariate analysis, patients with high iliac crests require longer OT and larger IBL when performing PETD (31). Notably, there were no statistically significant differences in ILH and ILW between the 2 subtypes obtained in our study. Therefore, PEID might be suitable for patients with both subtypes. However, PEID required traction of the nerve and the dural sac during the operation, which may consequently lead to complications such as nerve damage and dural tear. Also, PEID often requires general anesthesia due to the poor effect of local anesthesia (32,33). Due to the retrospective nature of our current study, we recorded the surgical approach that patient actually underwent as the “choice” of the surgeons as we considered that ultimately the surgeons choose this approach as being most appropriate based on their clinical experience. In the current study, after a thorough preoperative assessment of the patients according to the surgeon’s experience, about 68.9% (31/45) of patients with subtype 2 were chosen for PETD whereas 84.8% (56/66) of patients with subtype 1 were chosen for PEID. Furthermore, subgroup analysis revealed that patients undergoing PETD surgery exhibited lower ITW and IH, while presenting a larger ITH and foraminal sizes. These metrics were also crucial for identifying subtypes based on radiographic parameters. Similar to our clustering results, for patients exhibiting subtype 2 (e.g., lower ITW, IH and larger foraminal sizes), PETD is the preferable choice, disregarding the specific kind of disc herniation. Meanwhile, for subtype 1 (higher ITW, IH and smaller foraminal sizes), PEID is preferred. As far as we are aware, the current study is the first to utilize radiographic metrics to assess the relationship between the morphology pattern of lumbosacral region and surgical approaches. More studies are needed in the future to validate our results.
Limitations
This study had several limitations: (I) information from 3-dimensional computed tomography (CT) reconstruction could provide a more comprehensive view of the morphometry in the lumbosacral region; studies including CT analyses are needed in the future; (II) the sample size of dataset 2 which was used to explore the surgical-related information differences between subtypes was relatively small and long-term clinical and functional outcomes which of great importance to our model have not been assessed; (III) body mass index (BMI) is another important factor which affects the “ease” of spine surgery in clinical practice (34); however, it was not included due to the retrospective nature of our current study. In the future, we would thoroughly investigate the impact of BMI on the surgical choice of endoscopic spinal surgery; (IV) we focused on the impact of bone anatomy on surgical approach selection, and the type of disc herniation needs to be considered in future studies.
Conclusions
The morphology pattern of the lumbosacral region affects the ease of different PELD procedures when performing percutaneous discectomy at the segment of L5–S1. Without considering the type of disc herniation, this classification system might aid the spine surgeons for selecting appropriate surgical approach.
Acknowledgments
Funding: This work was supported by
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://qims.amegroups.com/article/view/10.21037/qims-23-277/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://qims.amegroups.com/article/view/10.21037/qims-23-277/coif). BX reports that this work was supported by the National Natural Science Foundation of China (Nos. 82072491 and 31900967), the Natural Science Foundation of Tianjin city (No. 20JCYBJC00820), and the Science and Technology Project of Tianjin Municipal Health Commission (No. KJ20211). The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Institutional Ethics Committee of Tianjin Hospital (No. 2023 medical ethical review 007). Written informed consent was provided by each participant prior to each procedure.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Benzakour T, Igoumenou V, Mavrogenis AF, Benzakour A. Current concepts for lumbar disc herniation. Int Orthop 2019;43:841-51. [Crossref] [PubMed]
- Yuan P, Shi X, Wei X, Wang Z, Mu J, Zhang H. Development process and clinical application of collagenase chemonucleolysis in the treatment of lumbar disc herniation: a narrative review in China. Postgrad Med J 2023. [Epub ahead of print]. pii: postgradmedj-2021-141208. doi:
10.1136/postmj/postgradmedj-2021-141208 . - Chen BL, Guo JB, Zhang HW, Zhang YJ, Zhu Y, Zhang J, Hu HY, Zheng YL, Wang XQ. Surgical versus non-operative treatment for lumbar disc herniation: a systematic review and meta-analysis. Clin Rehabil 2018;32:146-60. [Crossref] [PubMed]
- Pan M, Li Q, Li S, Mao H, Meng B, Zhou F, Yang H. Percutaneous Endoscopic Lumbar Discectomy: Indications and Complications. Pain Physician 2020;23:49-56.
- Kim M, Lee S, Kim HS, Park S, Shim SY, Lim DJ. A Comparison of Percutaneous Endoscopic Lumbar Discectomy and Open Lumbar Microdiscectomy for Lumbar Disc Herniation in the Korean: A Meta-Analysis. Biomed Res Int 2018;2018:9073460. [Crossref] [PubMed]
- Ahn Y. Endoscopic spine discectomy: indications and outcomes. Int Orthop 2019;43:909-16. [Crossref] [PubMed]
- Zhao Y, Yuan S, Tian Y, Liu X. Necessity of routinely performing foraminoplasty during percutaneous endoscopic transforaminal discectomy (PETD) for lumbar disc herniation. Br J Neurosurg 2023;37:277-83. [Crossref] [PubMed]
- Song QC, Zhao Y, Li D, Zhang YK, Fan LH, Li QY, Duan DP, Shi ZB. Percutaneous endoscopic transforaminal discectomy for the treatment of L5-S1 lumbar disc herniation and the influence of iliac crest height on its clinical effects. Exp Ther Med 2021;22:866. [Crossref] [PubMed]
- Mo X, Shen J, Jiang W, Zhang X, Zhou N, Wang Y, Hu Z, Hao J. Percutaneous Endoscopic Lumbar Diskectomy for Axillar Herniation at L5-S1 via the Transforaminal Approach Versus the Interlaminar Approach: A Prospective Clinical Trial. World Neurosurg 2019;125:e508-14. [Crossref] [PubMed]
- Choi KC, Park CK. Percutaneous Endoscopic Lumbar Discectomy for L5-S1 Disc Herniation: Consideration of the Relation between the Iliac Crest and L5-S1 Disc. Pain Physician 2016;19:E301-8.
- Chen J, Jing X, Li C, Jiang Y, Cheng S, Ma J. Percutaneous Endoscopic Lumbar Discectomy for L5S1 Lumbar Disc Herniation Using a Transforaminal Approach Versus an Interlaminar Approach: A Systematic Review and Meta-Analysis. World Neurosurg 2018;116:412-420.e2. [Crossref] [PubMed]
- Patgaonkar P, Datar G, Agrawal U, Palanikumar C, Agrawal A, Goyal V, Patel V. Suprailiac versus transiliac approach in transforaminal endoscopic discectomy at L5-S1: a new surgical classification of L5-iliac crest relationship and guidelines for approach. J Spine Surg 2020;6:S145-54. [Crossref] [PubMed]
- Wang C, Li C, Zhang R, Li Z, Zhang H, Zhang Y, Liu S, Chi X, Zhao R. Identification of radiographic characteristics associated with pain in hallux valgus patients: A preliminary machine learning study. Front Public Health 2022;10:943026. [Crossref] [PubMed]
- Zheng C, Wu F, Cai L. Transforaminal percutaneous endoscopic discectomy in the treatment of far-lateral lumbar disc herniations in children. Int Orthop 2016;40:1099-102. [Crossref] [PubMed]
- Babaee T, Kamyab M, Ahmadi A, Sanjari MA, Ganjavian MS. The intra- and inter-observer reliability of interface pressure measurements of the Milwaukee brace in adolescents with hyperkyphosis. J Back Musculoskelet Rehabil 2019;32:647-54. [Crossref] [PubMed]
- Ebraheim NA, Xu R, Huntoon M, Yeasting RA. Location of the extraforaminal lumbar nerve roots. An anatomic study. Clin Orthop Relat Res 1997;230-5. [Crossref] [PubMed]
- Ruetten S, Komp M, Godolias G. A New full-endoscopic technique for the interlaminar operation of lumbar disc herniations using 6-mm endoscopes: prospective 2-year results of 331 patients. Minim Invasive Neurosurg 2006;49:80-7. [Crossref] [PubMed]
- Hoogland T, Schubert M, Miklitz B, Ramirez A. Transforaminal posterolateral endoscopic discectomy with or without the combination of a low-dose chymopapain: a prospective randomized study in 280 consecutive cases. Spine (Phila Pa 1976) 2006;31:E890-7. [Crossref] [PubMed]
- Ahn Y, Lee SH, Park WM, Lee HY, Shin SW, Kang HY. Percutaneous endoscopic lumbar discectomy for recurrent disc herniation: surgical technique, outcome, and prognostic factors of 43 consecutive cases. Spine (Phila Pa 1976) 2004;29:E326-32. [Crossref] [PubMed]
- Dabo X, Ziqiang C, Yinchuan Z, Haijian N, Kai C, Yanbin L, Qiang F, Chuanfeng W. The Clinical Results of Percutaneous Endoscopic Interlaminar Discectomy (PEID) in the Treatment of Calcified Lumbar Disc Herniation: A Case-Control Study. Pain Physician 2016;19:69-76.
- Gao A, Yang H, Zhu L, Hu Z, Lu B, Jin Q, Wang Y, Gu X. Comparison of Interlaminar and Transforaminal Approaches for Treatment of L(5) /S(1) Disc Herniation by Percutaneous Endoscopic Discectomy. Orthop Surg 2021;13:63-70. [Crossref] [PubMed]
- Chen W, Zheng Y, Liang G, Chen G, Hu Y. Clinical effects of transforaminal approach vs interlaminar approach in treating lumbar disc herniation: A clinical study protocol. Medicine (Baltimore) 2020;99:e22701. [Crossref] [PubMed]
- Nie H, Zeng J, Song Y, Chen G, Wang X, Li Z, Jiang H, Kong Q. Percutaneous Endoscopic Lumbar Discectomy for L5-S1 Disc Herniation Via an Interlaminar Approach Versus a Transforaminal Approach: A Prospective Randomized Controlled Study With 2-Year Follow Up. Spine (Phila Pa 1976) 2016;41:B30-7. [Crossref] [PubMed]
- Huang Y, Yin J, Sun Z, Song S, Zhuang Y, Liu X, Du S, Rui Y. Percutaneous endoscopic lumbar discectomy for LDH via a transforaminal approach versus an interlaminar approach: a meta-analysis. Orthopade 2020;49:338-49. [Crossref] [PubMed]
- Yang H, Gao W, Duan Y, Kang X, He B, Hao D, Wang B. Two-dimensional fluoroscopy-guided robot-assisted percutaneous endoscopic transforaminal discectomy: a retrospective cohort study. Am J Transl Res 2022;14:3121-31.
- Ahn Y, Lee HY, Lee SH, Lee JH. Dural tears in percutaneous endoscopic lumbar discectomy. Eur Spine J 2011;20:58-64. [Crossref] [PubMed]
- Zhu K, He D. Transforaminal percutaneous endoscopic discectomy for symptomatic gas-filled discal cysts-report of three cases and literature review. J Orthop Surg Res 2021;16:251. [Crossref] [PubMed]
- Zhou C, Zhang G, Panchal RR, Ren X, Xiang H, Xuexiao M, Chen X, Tongtong G, Hong W, Dixson AD. Unique Complications of Percutaneous Endoscopic Lumbar Discectomy and Percutaneous Endoscopic Interlaminar Discectomy. Pain Physician 2018;21:E105-12.
- Hurday Y, Xu B, Guo L, Cao Y, Wan Y, Jiang H, Liu Y, Yang Q, Ma X. Radiographic measurement for transforaminal percutaneous endoscopic approach (PELD). Eur Spine J 2017;26:635-45. [Crossref] [PubMed]
- Li X, Hu Z, Cui J, Han Y, Pan J, Yang M, Tan J, Sun G, Li L. Percutaneous endoscopic lumbar discectomy for recurrent lumbar disc herniation. Int J Surg 2016;27:8-16. [Crossref] [PubMed]
- Sun DD, Lv D, Wu WZ, Ren HF, Bao BH, Liu Q, Sun ML. Estimation and influence of blood loss under endoscope for percutaneous endoscopic lumbar discectomy (PELD): a clinical observational study combined with in vitro experiment. J Orthop Surg Res 2020;15:281. [Crossref] [PubMed]
- Hua W, Tu J, Li S, Wu X, Zhang Y, Gao Y, Zeng X, Yang S, Yang C. Full-endoscopic discectomy via the interlaminar approach for disc herniation at L4-L5 and L5-S1: An observational study. Medicine (Baltimore) 2018;97:e0585. [Crossref] [PubMed]
- Wang D, Xie W, Cao W, He S, Fan G, Zhang H. A Cost-utility Analysis of Percutaneous Endoscopic Lumbar Discectomy for L5-S1 Lumbar Disc Herniation: Transforaminal versus Interlaminar. Spine (Phila Pa 1976) 2019;44:563-70. [Crossref] [PubMed]
- Rushton AB, Jadhakhan F, Verra ML, Emms A, Heneghan NR, Falla D, Reddington M, Cole AA, Willems PC, Benneker L, Selvey D, Hutton M, Heymans MW, Staal JB. Predictors of poor outcome following lumbar spinal fusion surgery: a prospective observational study to derive two clinical prediction rules using British Spine Registry data. Eur Spine J 2023;32:2303-18. [Crossref] [PubMed]



