
Quantifying carotid stiffness in chronic kidney disease using ultrafast ultrasound imaging
Introduction
The morbidity, mortality, and disability associated with chronic kidney disease (CKD), a global public health problem, have increased significantly with the aging population (1). Several studies have reported a high incidence of cardiovascular diseases in CKD patients (2-4). Experiments in mice have demonstrated that CKD greatly accelerates the progression of atherosclerosis (3). CKD is often accompanied by pathophysiological conditions, such as inflammation and oxidative stress, that damage smooth muscle and endothelial cells, cause vascular calcifications (4,5), and increase arterial stiffness (6). Intimal and intermediate calcifications are associated with renal function decline in CKD patients (7). Early intervention can reduce global morbidity, cardiovascular mortality, and all-cause mortality in CKD patients (8). Clinical biochemical indicators of renal function often only increase in advanced stages of CKD. Therefore, there is an urgent need for reliable indicators of atherosclerosis in early CKD.
Carotid intima-media thickness (cIMT) can be used as a predictor for cardiovascular events and death in CKD patients on dialysis (9). Increased cIMT may indicate declining renal function in early stages of CKD (10). However, cIMT measured using ultrasonography is highly operator-dependent and lacks standardization, resulting in unstable measurements and poor reproducibility (11). Moreover, recent studies have demonstrated that cIMTs in CKD patients were similar to those without a history of CKD (0.78±0.21 and 0.65±0.16 mm, respectively, P=0.11) (12). In addition, increased cIMT is a morphological change; it is functional carotid artery stiffness, caused by vascular endothelial dysfunction, that occurs in the early stages of CKD (13). Consequently, it is important to find reliable indicators to reflect early pathological changes in the carotid arteries of CKD patients.
Pulse wave velocity (PWV) can be used for visual assessment of atherosclerosis and was recommended as the gold standard in the 2018 European Society of Cardiology/European Society of Hypertension guidelines for the management of arterial hypertension (14). Previous PWV techniques, such as cervical-femoral PWV, showed significantly increased central arterial stiffness in stage 3B CKD. Meanwhile, cervical-radial PWV, which reflects peripheral arterial stiffness, did not show these findings (15). Distinct from all those PWV techniques, ultrafast PWV (ufPWV) is a unique PWV technology that directly records the propagation of carotid pulse wave via ultra-fast instantaneous ultrasonography in real-time assessment (>2,000 frame/s) (16). ufPWV can indirectly evaluate the stiffness of the straight carotid in vivo and quantitatively reflect the degree of systemic atherosclerosis (17). In recent years, ufPWV has been used for the evaluation of pre-hypertension (16), coronary artery disease (17), diabetes (18), and valvular heart disease (19). Previous studies validated the stability and reproducibility of ufPWV and confirmed its utility in subclinical atherosclerosis (20,21). However, the use of ufPWV in CKD has not yet been reported.
The present study explored the association between carotid stiffening, quantified using ufPWV, and renal function injury, and developed an indicator for early renal damage. We present this article in accordance with the STROBE reporting checklist (available at https://qims.amegroups.com/article/view/10.21037/qims-23-503/rc).
Methods
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committee of the Affiliated Hospital of Nanjing University of Chinese Medicine (No. 2017NL-048-02) and the requirement for individual consent for this retrospective analysis was waived.
Study design and participants
Between March 2017 and May 2022, 582 participants aged 19–80 years were enrolled in this retrospective study. The sample included outpatients (62%) and inpatients (38%) from the geriatric (26%), cardiology (57%), and nephrology (17%) departments of the Affiliated Hospital of Nanjing University of Traditional Chinese Medicine. The patients underwent ufPWV examination and baseline data collection, including clinical interviews, physical examinations, and laboratory investigations. The CKD Epidemiological Cooperation equation was used to calculate the estimated glomerular filtration rate (eGFR) (22). CKD was divided into 5 stages according to eGFR by the Kidney Disease Outcomes Quality Initiative (K/DOQI) expert group of the American Nephrology Foundation (23). Patients who met any of the following conditions were excluded: (I) lack of complete data (including serum creatinine and serum urea; n=59); (II) invalid ufPWV measurements (detailed in the carotid ultrasonography section; n=148); (III) clinical conditions that could affect PWV reliability, including body mass index (BMI) ≥40 kg/m2 (n=15) and severe arrhythmias (n=4); and (IV) dialysis patients (n=58). After exclusion of these patients, a total of 298 (51.2%) participants were included. The control group included 205 (35.2%) patients without a history of CKD and eGFR ≥90 mL/min/1.73 m2 (100 males and 105 females; average age, 51.96±10.37 years). Stages 1 (n=28) and 2 (n=16) CKD patients were included in the early CKD group (n=44), whereas stages 3 (n=12), 4 (n=21), and 5 (n=16) patients were included in the advanced CKD group (n=49) (Figure 1, Table 1).

Table 1
| Variables | Total (n=298) | Controls (n=205) | Early CKD (n=44) | Advanced CKD (n=49) | P value |
|---|---|---|---|---|---|
| Baseline characteristics | |||||
| Age (years) | 52.49±11.05 | 51.96±10.37 | 51.48±12.38 | 55.63±12.17 | 0.090 |
| Male | 151 (50.7) | 100 (48.8) | 22 (50.0) | 29 (59.2) | 0.423 |
| BMI (kg/m2) | 24.34±3.30 | 24.15±2.92 | 25.73±3.99 | 23.90±3.81 | 0.009 |
| CKD duration (years) | 7.19±8.92 | – | 4.65±8.84 | 9.48±8.45 | 0.008 |
| Hypertension | 179 (60.1) | 128 (62.4) | 13 (29.5) | 38 (77.6) | <0.001 |
| Diabetes | 29 (9.7) | 5 (2.4) | 11 (25.0) | 13 (26.5) | <0.001 |
| Smokers | 68 (22.8) | 44 (21.5) | 14 (31.8) | 10 (20.4) | 0.301 |
| SBP (mmHg) | 132.67±17.85 | 129.34±15.66 | 131.77±13.46 | 147.41±22.30 | <0.001 |
| DBP (mmHg) | 81.34±11.48 | 81.10±11.42 | 80.43±10.42 | 83.18±12.64 | 0.444 |
| BPM use | 161 (54.0) | 126 (61.5) | 10 (22.7) | 25 (51.0) | <0.001 |
| Statin use | 85 (28.5) | 51 (24.9) | 20 (45.5) | 14 (28.6) | 0.023 |
| Laboratory findings | |||||
| TC (mmol/L) | 4.91±1.17 | 4.90±0.95 | 5.18±1.36 | 4.75±1.70 | 0.190 |
| TG (mmol/L) | 1.68±1.28 | 1.52±1.18 | 1.94±1.58 | 2.13±1.27 | 0.004 |
| LDL (mmol/L) | 2.74±0.78 | 2.79±0.77 | 2.62±0.75 | 2.60±0.82 | 0.162 |
| HDL (mmol/L) | 1.48±0.34 | 1.54±0.33 | 1.35±0.36 | 1.32±0.27 | <0.001 |
| FBG (mmol/L) | 5.47±1.08 | 5.39±0.74 | 5.61±1.29 | 5.73±1.83 | 0.092 |
| Cr (µmol/L) | 113.30±152.14 | 68.60±13.92 | 75.08±19.33 | 334.60±286.70 | <0.001 |
| eGFR (mL/min/1.73 m2) | 126.45±43.59 | 144.15±18.66 | 134.20±25.76 | 45.45±39.90 | <0.001 |
Data are presented as mean ± standard deviation or n (%). CKD, chronic kidney disease; BMI, body mass index; SBP, systolic blood pressure; DBP, diastolic blood pressure; BPM, blood pressure medication; TC, total cholesterol; TG, triglyceride; LDL, low-density lipoprotein; HDL, high-density lipoprotein; FBG, fasting blood glucose; Cr, creatinine; eGFR, estimated glomerular filtration rate.
Carotid ultrasonography
The Aixplorer ultrafast commercial scanner (SuperSonic Imagine, Aix-en-Provence, France) was used to determine the cIMT and ufPWV with a linear array probe SL10-2 (frequency: 2–10 MHz; center frequency: 8.0 MHz). In the supine position, the neck was fully exposed and relaxed, and the head was turned to one side. In mode B, the common carotid artery was scanned longitudinally to obtain a clear sonogram of the intima-media. cIMT measurements were performed after image optimization. The measurement system was used to determine the sampling frame, with a fixed width of 1.0 cm, to automatically track and record posterior wall cIMT of the distal segment of common carotid artery (1.0–1.5 cm below the carotid bulb). The ratio, obtained by dividing the length of cIMT segment by the sampling frame width, was used as a quality control index; measurements >70% were considered valid (Figure 2A). Each carotid was measured 3 times and the average was calculated. The average value for both sides was then calculated to obtain the final value.

The participants were then instructed to hold their breath and the “PWV” key was pressed to activate ultrafast imaging acquisition, which was completed within 3 seconds. After obtaining a stable ufPWV image, a region of interest (ROI) was selected and adjusted to cover a section of the common carotid artery. The software automatically recorded the PWV at the beginning of systole (PWV-BS) and PWV at the end of systole (PWV-ES) with their respective standard deviations (SDs) (denoted by Δ±; Figure 2B). For quality control, Δ± ≤2.0 m/s was considered valid for ufPWV acquisition. Invalid measurements included those with (I) failure to calculate PWV-BS or PWV-ES; (II) Δ± of >2.0 m/s; and (III) improper ROI localization with the tracing line outside of the arterial wall (20,21). The means of three valid PWV-BS and PWV-ES values for bilateral common carotid arteries were taken as their respective final values.
Statistical analysis
Continuous variables were expressed as mean ± SD, whereas categorical variables were expressed as counts and ratios. One-way analysis of variance (ANOVA) and chi-square test were used to compare the continuous and categorical variables of participant characteristics between groups in total, respectively. The least significant difference (LSD) test was further used to compare cIMT, PWV-BS, and PWV-ES between groups in pairs, respectively. Pearson’s correlation analysis was used to analyze the relationships among ultrasound characteristics (cIMT, PWV-BS, PWV-ES) and major cardiovascular risk factors [including age, BMI, CKD duration, systolic blood pressure (SBP), diastolic blood pressure (DBP), total cholesterol (TC), triglyceride (TG), low-density lipoprotein (LDL), high-density lipoprotein (HDL), fasting blood glucose (FBG), and eGFR]. Scatter plots and subgroups correlation analysis were used to determine the correlated r for each group of cIMT, PWV-BS, and PWV-ES, linked to age. Statistical analyses were performed using the software SPSS 22.0 (IBM Corp., Armonk, NY, USA), and two-sided P<0.05 was considered statistically significant.
Results
Participant characteristics
The early CKD group included 22 males and 22 females (average age, 51.48±12.38 years), whereas the advanced CKD group included 29 males and 20 females (average age, 55.63±12.17 years). Baseline demographic, clinical, and laboratory characteristics are summarized in Table 1. All clinical measurements except for age, male sex, smoking, and DBP differed significantly according to CKD status. Similarly, significant differences were found in major serum biomarkers except for TC, LDL, and FBG. Cases in the advanced CKD subgroup demonstrated a remarkable increase in creatinine and CKD duration, and decrease in eGFR compared with cases in the control and early CKD subgroups (P<0.001 in total and P<0.001 for all pairwise comparisons).
Comparison of cIMT and carotid stiffening
For decades, ultrasonic imaging characteristics such as cIMT, which is currently a surrogate measure for atherosclerosis, were frequently used to identify early atherosclerosis, and to predict future cardiovascular events. In this study, there were no significant overall differences in cIMT among the control, early CKD, and advanced CKD groups (P=0.240), but the overall significant differences were found in both PWV-BS and PWV-ES, as shown in Table 2 (P=0.002 and P<0.001). Pairwise comparisons showed no significant differences in cIMT (P=0.092, 0.796, and 0.249 for controls vs. early CKD, early vs. advanced CKD, and controls vs. advanced CKD, respectively; Figure 3A). The PWV-BS and PWV-ES for early and advanced CKD groups were significantly higher than those for controls (P=0.002 and 0.024 for PWV-BS; P=0.023 and P<0.001 for PWV-ES; Table 2, Figure 3B,3C), but there was no significant difference between the early and advanced CKD groups (P=0.419 for PWV-BS; P=0.153 for PWV-ES; Table 2, Figure 3B,3C).
Table 2
| Variables | Controls (n=205) |
Early CKD (n=44) |
Advanced CKD (n=49) |
Comparing in total |
Controls vs. early CKD |
Early vs. advanced CKD |
Controls vs. advanced CKD |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| F value | P value | SE | P value | SE | P value | SE | P value | |||||||
| cIMT (cm) | 0.060±0.012 | 0.057±0.014 | 0.060±0.012 | 1.433 | 0.240 | 0.0020 | 0.092 | 0.0025 | 0.796 | 0.0019 | 0.249 | |||
| PWV-BS (m/s) | 5.73±1.07 | 6.33±1.34 | 6.14±1.19 | 6.499 | 0.002 | 0.1884 | 0.002 | 0.2355 | 0.419 | 0.1803 | 0.024 | |||
| PWV-ES (m/s) | 8.09±1.69 | 8.77±1.85 | 9.29±2.07 | 10.250 | <0.001 | 0.2954 | 0.023 | 0.3692 | 0.153 | 0.2827 | <0.001 | |||
Data are mean ± standard deviation. CKD, chronic kidney disease; SE, standard error; cIMT, carotid intima-media thickness; PWV-BS, pulse wave velocity at the beginning of systole; PWV-ES, pulse wave velocity at the end of systole.

Correlation analysis of cIMT, PWV-BS, PWV-ES, and cardiovascular risk factors
Atherosclerosis is a lifelong disease process that progresses slowly at a young age and may accelerate with the accumulation of numerous cardiovascular risk factors. Among those risk factors, age (r=0.408, P<0.001), BMI (r=0.254, P<0.001), SBP (r=0.210, P<0.001), DBP (r=0.140, P=0.016), LDL (r=0.195, P=0.001), and FBG (r=0.251, P<0.001) correlated significantly with cIMT. PWV-BS only correlated significantly with age (r=0.158, P=0.006) and eGFR (r=−0.128, P=0.027). PWV-ES correlated significantly with age (r=0.474, P<0.001), SBP (r=0.211, P<0.001), FBG (r=0.154, P=0.008), and eGFR (r=−0.188, P=0.001); the correlation was the greatest with age (Table 3).
Table 3
| Variables | cIMT | PWV-BS | PWV-ES | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| r value | Covariance | P value | r value | Covariance | P value | r value | Covariance | P value | |||
| Age (years) | 0.408 | 0.054 | <0.001† | 0.158 | 2.018 | 0.006† | 0.474 | 9.599 | <0.001† | ||
| BMI (kg/m2) | 0.254 | 0.010 | <0.001† | 0.077 | 0.293 | 0.185 | 0.041 | 0.247 | 0.481 | ||
| CKD duration (years) | 0.095 | 0.011 | 0.363 | −0.089 | −1.004 | 0.394 | 0.045 | 0.788 | 0.671 | ||
| SBP (mmHg) | 0.210 | 0.045 | <0.001† | 0.025 | 0.511 | 0.670 | 0.211 | 6.907 | <0.001† | ||
| DBP (mmHg) | 0.140 | 0.019 | 0.016† | 0.026 | 0.034 | 0.660 | 0.071 | 1.492 | 0.222 | ||
| TC (mmol/L) | 0.091 | 0.001 | 0.117 | −0.017 | −0.022 | 0.775 | −0.102 | −0.218 | 0.079 | ||
| TG (mmol/L) | −0.012 | <0.001 | 0.842 | −0.051 | −0.075 | 0.382 | −0.021 | −0.050 | 0.715 | ||
| LDL (mmol/L) | 0.195 | 0.002 | 0.001† | −0.025 | −0.022 | 0.671 | −0.053 | −0.076 | 0.359 | ||
| HDL (mmol/L) | −0.001 | <0.001 | 0.989 | 0.013 | 0.005 | 0.818 | −0.068 | −0.042 | 0.243 | ||
| FBG (mmol/L) | 0.251 | 0.003 | <0.001† | 0.098 | 0.123 | 0.090 | 0.154 | 0.306 | 0.008† | ||
| eGFR (mL/min/1.73 m2) | 0.005 | 0.003 | 0.930 | −0.128 | −6.438 | 0.027† | −0.188 | −15.040 | 0.001† | ||
†, significant P values at <0.05. cIMT, carotid intima-media thickness; PWV-BS, pulse wave velocity at the beginning of systole; PWV-ES, pulse wave velocity at the end of systole; BMI, body mass index; CKD, chronic kidney disease; SBP, systolic blood pressure; DBP, diastolic blood pressure; TC, total cholesterol; TG, triglyceride; LDL, low-density lipoprotein; HDL, high-density lipoprotein; FBG, fasting blood glucose; eGFR, estimated glomerular filtration rate.
Correlation analysis of cIMT, PWV-BS, PWV-ES, and age
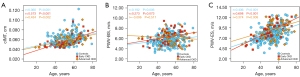
As we all know, age is the dominant driver of atherosclerosis, cardiovascular risk factors, and cardiovascular events. cIMT increased with age in all three groups, with the strongest correlation for early CKD group, followed by advanced CKD and control groups (r=0.573, P<0.001; r=0.434, P=0.002; and r=0.360, P<0.001, respectively) (Figure 4A). PWV-BS did not correlate significantly with age in the early and advanced CKD groups (all P>0.05), but had a weak positive correlation in controls (r=0.192, P=0.006) (Figure 4B). PWV-ES also increased with age, with the strongest correlation for the early CKD group, followed by the control and advanced CKD groups (r=0.698, P<0.001; r=0.436, P<0.001; and r=0.374, P=0.008, respectively) (Figure 4C).
Discussion
CKD accelerates the progression of atherosclerosis, which leads to increased mortality (24). It has been demonstrated that atherosclerosis of large arteries begins in the early stages of CKD, when renal function is only slightly reduced (13). In CKD patients with decreased renal function, PWV may be used to assess the cardiovascular risk and predict CKD progression and mortality (25). Our previous studies validated satisfactory intra- and inter-operator reproducibility of ufPWV measurements (20,21), and demonstrated that the ufPWV parameter, PWV-ES, can be used for early diagnosis and quantitative assessment of the degree of atherosclerosis (20), and to identify carotid atherosclerosis in healthy adults without major cardiovascular risk factors (21). Consistent with previous studies (13,20,25), our findings indicate that PWV-ES is significantly higher in early CKD patients than in controls (P<0.05), and has a significantly positive correlation with age in all three groups. However, the correlated r of PWV-ES linked to age were higher than those of cIMT in the control and early CKD populations, yet lower in advanced CKD. The increase in arterial stiffness begins in the early stages of CKD and slows down in the progressive stages. This is perhaps because an increase in arterial stiffness might not unendingly correlate with continuously increasing cIMT (20,21), and indicates that ufPWV might be a quantitative tool more suitable for assessing early atherosclerosis in CKD.
Ageing is the dominant driver of carotid stiffening and atherosclerosis, which promotes the rupture of elastin fibers in arterial walls and increases collagen accumulation, leading to arteriosclerosis (26). Li et al. (27) found that carotid PWV increased with age in CKD patients, but was alleviated in patients who underwent kidney transplantation after removal of major atherosclerotic risk factors, such as chronic renal insufficiency and arteriovenous fistulae. An analysis of end-stage renal disease patients by Tripepi et al. (28) demonstrated that the correlation between PWV and cardiovascular events was greater in younger ages. Our previous study using ufPWV confirmed a strong positive correlation between age and arterial stiffness, represented by PWV-ES (r=0.710) (20). The results of the present study were consistent with previous studies (20,26-28), and it further demonstrated that CKD patients had greater arterial stiffness, which was most strongly correlated with age in the early stages (r=0.698, P<0.001). Besides, PWV-ES performed better than PWV-BS at assessing age-related atherosclerosis in prior and our studies (20,21). This is probably due to differences in the wall recoil during the cardiac cycle, since early systolic expansions powered by left ventricular ejection may hinder detection of minute differences in wall stiffness. Therefore, PWV-ES may be used to evaluate age-related decrease in arterial elasticity in healthy individuals and CKD patients.
A histopathological study (18) suggested that the increase in intima-media thickness may be mainly due to lipid deposition in the intima and outward migration of smooth muscle cells, which leads to collagen proliferation, reduced elastin, and increased vascular stiffness. Previous studies (29-31) have indicated that eGFR is negatively correlated with cIMT and PWV, potentially damaging the structure and function of large blood vessels in CKD patients. Meanwhile, another study (32) found that cIMT had a limited role in the assessment of structural and functional vascular abnormalities in different stages of CKD. Although cIMT increases with age, it lags behind ufPWV as an indicator for age-related atherosclerosis (20). The present study also demonstrated that cIMT correlates positively with age (r=0.408, P<0.001), and may be influenced by various atherosclerosis risk factors. However, there were no significant differences among different stages of CKD, which was consistent with the results of previous studies (20,32). This is because cIMT, the traditional index for structural atherosclerosis, changes later than ufPWV.
This study had some limitations. First, the single-center study had a small sample size, and further multi-center studies may be needed to validate these findings. Second, even comprehensive adjustments cannot eliminate the role of confounding factors, including poor lifestyle, medication use, and concomitant tumors, in observational clinical studies. Although CKD may be caused by diabetes, the influence of hyperglycemia on carotid stiffness cannot be ruled out. Third, CKD patients, particularly those in middle and advanced stages, are often hypertensive, which itself is a strong risk factor for atherosclerosis. Fourth, almost a quarter of cases (25.4%, 148/582) had an invalid ufPWV measurement in this study, which likely reflects predictable challenges when introducing this new technology for CKD assessment. Finally, it should be noted that this study was conducted on subgroups through correlation analysis and hence the possibility of the effect of nonlinear and multivariate regression relationships on carotid properties was not considered in this study.
Conclusions
ufPWV can be used to quantitatively assess carotid stiffness in CKD patients and predict the risk of atherosclerosis. PWV-ES may be superior to PWV-BS and cIMT for the assessment of carotid atherosclerosis in early CKD patients.
Acknowledgments
Funding: This work was supported by grants from
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://qims.amegroups.com/article/view/10.21037/qims-23-503/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://qims.amegroups.com/article/view/10.21037/qims-23-503/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committee of the Affiliated Hospital of Nanjing University of Chinese Medicine (No. 2017NL-048-02) and the requirement for individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Hu J, Ke R, Teixeira W, Dong Y, Ding R, Yang J, Ai X, Ye DW, Shang J. Global, Regional, and National Burden of CKD due to Glomerulonephritis from 1990 to 2019: A Systematic Analysis from the Global Burden of Disease Study 2019. Clin J Am Soc Nephrol 2023;18:60-71. [Crossref] [PubMed]
- Zietzer A, Steffen E, Niepmann S, Düsing P, Hosen MR, Liu W, Jamme P, Al-Kassou B, Goody PR, Zimmer S, Reiners KS, Pfeifer A, Böhm M, Werner N, Nickenig G, Jansen F. MicroRNA-mediated vascular intercellular communication is altered in chronic kidney disease. Cardiovasc Res 2022;118:316-33. [Crossref] [PubMed]
- Mathew AV, Zeng L, Atkins KB, Sadri KN, Byun J, Fujiwara H, Reddy P, Pennathur S. Deletion of bone marrow myeloperoxidase attenuates chronic kidney disease accelerated atherosclerosis. J Biol Chem 2021;296:100120. [Crossref] [PubMed]
- Ren SC, Mao N, Yi S, Ma X, Zou JQ, Tang X, Fan JM. Vascular Calcification in Chronic Kidney Disease: An Update and Perspective. Aging Dis 2022;13:673-97. [Crossref] [PubMed]
- Viegas C, Araújo N, Marreiros C, Simes D. The interplay between mineral metabolism, vascular calcification and inflammation in Chronic Kidney Disease (CKD): challenging old concepts with new facts. Aging (Albany NY) 2019;11:4274-99. [Crossref] [PubMed]
- Georgianos PI, Vaios V, Eleftheriadis T, Zebekakis PE, Liakopoulos V. Pulse Wave Velocity Assessment for Cardiovascular Risk Prognostication in ESKD: Weighting Recent Evidence. Curr Vasc Pharmacol 2021;19:4-11. [Crossref] [PubMed]
- Zhang YX, Tang RN, Wang LT, Liu BC. Role of crosstalk between endothelial cells and smooth muscle cells in vascular calcification in chronic kidney disease. Cell Prolif 2021;54:e12980. [Crossref] [PubMed]
- Shlipak MG, Tummalapalli SL, Boulware LE, Grams ME, Ix JH, Jha V, Kengne AP, Madero M, Mihaylova B, Tangri N, Cheung M, Jadoul M, Winkelmayer WC, Zoungas S. Kidney Int 2021;99:34-47. [Crossref] [PubMed]
- Ohtake T, Kobayashi S. Chronic Kidney Disease and Atherosclerosis: An Important Implication of Carotid Intima-Media Thickness. J Atheroscler Thromb 2021;28:471-3. [Crossref] [PubMed]
- Kawada T. Carotid intima-media thickness and cardiovascular risk in patients with diabetes mellitus type 2 and chronic kidney disease. Ren Fail 2020;42:314. [Crossref] [PubMed]
- Willeit P, Tschiderer L, Allara E, Reuber K, Seekircher L, Gao L, et al. Carotid Intima-Media Thickness Progression as Surrogate Marker for Cardiovascular Risk: Meta-Analysis of 119 Clinical Trials Involving 100 667 Patients. Circulation 2020;142:621-42. [Crossref] [PubMed]
- Donderski R, Stróżecki P, Sulikowska B, Grajewska M, Trafny R, Bodnar M, Marszałek A, Stefańska A, Siódmiak J, Odrowąż-Sypniewska G, Manitius J. Assessment of Peritoneal Membrane Arteriolar Structure in Conjunction with Traditional Cardiovascular System Evaluation in Chronic Kidney Disease (CKD) Stage 5 Patients. Kidney Blood Press Res 2018;43:1042-52. [Crossref] [PubMed]
- Zanoli L, Empana JP, Perier MC, Alivon M, Ketthab H, Castellino P, Laude D, Thomas F, Pannier B, Laurent S, Jouven X, Boutouyrie P. Increased carotid stiffness and remodelling at early stages of chronic kidney disease. J Hypertens 2019;37:1176-82. [Crossref] [PubMed]
- Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens 2018;36:1953-2041. [Crossref] [PubMed]
- Zanoli L, Lentini P, Boutouyrie P, Fatuzzo P, Granata A, Corrao S, Gaudio A, Inserra G, Rapisarda F, Rastelli S, Laurent S, Malatino LS, Castellino P. Pulse wave velocity differs between ulcerative colitis and chronic kidney disease. Eur J Intern Med 2018;47:36-42. [Crossref] [PubMed]
- Ma X, Zhu Z, Wang Y, Shen B, Jiang X, Liu W, Wu Y, Zou C, Luan Y, Gao H, Huang H. Quantifying carotid stiffness in a pre-hypertensive population with ultrafast ultrasound imaging. Ultrasonography 2023;42:89-99. [Crossref] [PubMed]
- Li Y, Zhang Y, Geng X, Zhao S, Sun YX, Wang YB. Increased carotid stiffness detected by ultrafast ultrasound imaging is associated with the Gensini score. Med Ultrason 2020;22:183-8. [Crossref] [PubMed]
- Pan FS, Xu M, Yu L, Luo J, Li MY, Liang JY, Zheng YL, Xie XY. Relationship between carotid intima-media thickness and carotid artery stiffness assessed by ultrafast ultrasound imaging in patients with type 2 diabetes. Eur J Radiol 2019;111:34-40. [Crossref] [PubMed]
- Goudot G, Mirault T, Khider L, Pedreira O, Cheng C, Porée J, Gruest M, Jeunemaître X, Pernot M, Messas E. Carotid Stiffness Assessment With Ultrafast Ultrasound Imaging in Case of Bicuspid Aortic Valve. Front Physiol 2019;10:1330. [Crossref] [PubMed]
- Zhu ZQ, Chen LS, Wang H, Liu FM, Luan Y, Wu LL, Liu N, Wang P, Huang H. Carotid stiffness and atherosclerotic risk: non-invasive quantification with ultrafast ultrasound pulse wave velocity. Eur Radiol 2019;29:1507-17. [Crossref] [PubMed]
- Zhu ZQ, Chen LS, Jiang XZ, Wu YY, Zou C, Luan Y, Gao H, Dai P, Ma XH, Wu LL, Sun HJ, Wang YP, Zou F, Liu FM, Huang H. Absent atherosclerotic risk factors are associated with carotid stiffening quantified with ultrafast ultrasound imaging. Eur Radiol 2021;31:3195-206. [Crossref] [PubMed]
- Meeusen JW, Kasozi RN, Larson TS, Lieske JC. Clinical Impact of the Refit CKD-EPI 2021 Creatinine-Based eGFR Equation. Clin Chem 2022;68:534-9. [Crossref] [PubMed]
- Engelbertz C, Reinecke H, Breithardt G, Schmieder RE, Fobker M, Fischer D, Schmitz B, Pinnschmidt HO, Wegscheider K, Pavenstädt H, Brand E. Two-year outcome and risk factors for mortality in patients with coronary artery disease and renal failure: The prospective, observational CAD-REF Registry. Int J Cardiol 2017;243:65-72. [Crossref] [PubMed]
- Düsing P, Zietzer A, Goody PR, Hosen MR, Kurts C, Nickenig G, Jansen F. Vascular pathologies in chronic kidney disease: pathophysiological mechanisms and novel therapeutic approaches. J Mol Med (Berl) 2021;99:335-48. [Crossref] [PubMed]
- Townsend RR, Anderson AH, Chirinos JA, Feldman HI, Grunwald JE, Nessel L, Roy J, Weir MR, Wright JT Jr, Bansal N, Hsu CYCRIC Study Investigators. Association of Pulse Wave Velocity With Chronic Kidney Disease Progression and Mortality: Findings From the CRIC Study (Chronic Renal Insufficiency Cohort). Hypertension 2018;71:1101-7. [Crossref] [PubMed]
- Uejima T, Dunstan FD, Arbustini E, Łoboz-Grudzień K, Hughes AD, Carerj S, Favalli V, Antonini-Canterin F, Vriz O, Vinereanu D, Zamorano JL, Popescu BA, Evangelista A, Lancellotti P, Lefthériotis G, Kozakova M, Palombo C, Fraser AG. E-Tracking International Collaboration Group (ETIC). Age-specific reference values for carotid arterial stiffness estimated by ultrasonic wall tracking. J Hum Hypertens 2020;34:214-22. [Crossref] [PubMed]
- Li Z, Qin Y, Du L, Luo X. An improvement of carotid intima-media thickness and pulse wave velocity in renal transplant recipients. BMC Med Imaging 2018;18:23. [Crossref] [PubMed]
- Tripepi G, Agharazii M, Pannier B, D'Arrigo G, Mallamaci F, Zoccali C, London G. Pulse Wave Velocity and Prognosis in End-Stage Kidney Disease. Hypertension 2018;71:1126-32. [Crossref] [PubMed]
- Zuo J, Hu Y, Chang G, Chu SL, Tan I, Butlin M, Avolio A. Relationship between arterial stiffness and chronic kidney disease in patients with primary hypertension. J Hum Hypertens 2020;34:577-85. [Crossref] [PubMed]
- Xiong J, Qian Y, Yu S, Ji H, Teliewubai J, Chi C, Lu Y, Zhou Y, Fan X, Li J, Blacher J, Zhang Y, Xu Y. Somatotype and Its Impact on Asymptomatic Target Organ Damage in the Elderly Chinese: The Northern Shanghai Study. Clin Interv Aging 2021;16:887-95. [Crossref] [PubMed]
- Chisalita SI, Wijkman M, Davidson LT, Spångeus A, Nyström F, Östgren CJ. Toe brachial index predicts major acute cardiovascular events in patients with type 2 diabetes independently of arterial stiffness. Diabetes Res Clin Pract 2020;161:108040. [Crossref] [PubMed]
- Asp AM, Wallquist C, Rickenlund A, Hylander B, Jacobson SH, Caidahl K, Eriksson MJ. Aspects of carotid structure and function in health and different stages of chronic kidney disease. Clin Physiol Funct Imaging 2018;38:402-8. [Crossref] [PubMed]


