
Tissue-induced winding of permanent pacemaker passive-fixation leads
Introduction
The aging population and the increased survival rate of patients with heart diseases who may require pacemakers have led to a significant increase in implantation rates. According to a recent estimate, the number of patients receiving pacemaker implantation has steadily increased, with an annual implantation rate of 1 million (1). Permanent pacemaker implantation is the therapy choice for treating severe or symptomatic bradyarrhythmias, among which, sinus node dysfunction (SND) and high-degree atrioventricular block (AVB) are the most common indications (2).
The complications associated with permanent pacemaker implantation include pocket hematoma, infections, lead dislodgement/dysfunction, stroke, atrial fibrillation, myocardial infarction, heart failure, lead displacement or failure, pneumothorax, and death (1,3,4). The implantation of fixation leads is a critical part of the procedure; lead displacement or winding might occur after permanent pacemaker implantation (5,6), whereas leads winding during the procedure has never been reported. Here, we report a case of tissue-induced winding of permanent pacemaker passive-fixation leads during the procedure of permanent pacemaker implantation.
Case presentation
A 63-year-old man was admitted with a 1-week history of palpitation. He had a history of hypertension, myocardial infarction, and type 2 diabetes. A 24-hour ambulatory electrocardiograph confirmed the diagnosis of sick sinus syndrome (SSS) (Figure 1A). After clinical evaluation, we proposed implanting a dual-chamber permanent pacemaker (Boston Scientific, Marlborough, MA, USA) to mitigate clinical symptoms.
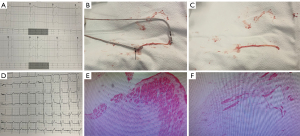
A temporary pacing electrode was placed in the apex of right ventricle before permanent pacemaker implantation. Then, two 7F sheaths were inserted into the left subclavian vein and a guide wire was successfully placed. A ventricular passive-fixation lead (Medtronic, Minneapolis, MN, USA) was placed in the bottom of the right ventricle. We then attempted to place the atrial passive-fixation lead into the right atrium, strangely, when the atrial lead was positioned in the right atrium, the ventricular and atrial leads were found to be fixed together by something (Video 1). Fluoroscopy demonstrated that the ventricular and atrial leads were closely connected, and we were unable to separate them (Video 2). We carefully retracted the ventricular and atrial leads simultaneously until they were placed in the puncture site of the left subclavian vein (Video 3). The ventricular fixation lead was then retracted from the subclavian vein with relatively substantial force, consequently, the head of ventricular fixation lead was removed and remained in the subclavian vein during the retracting process, as shown in Video 4. Upon careful retraction of the atrial lead outside of the subclavian vein, a mass of tissue with unknown origin was found attached on the head of atrial lead, and the head of ventricular lead was attached on the other side of the tissue. Figure 1B simulates the relative position of ventricular lead-tissue-atrial lead. The shape of the tissue is shown Figure 1C; the tissue was sent for pathological examination [hematoxylin-eosin (HE) staining]. Another new ventricular and atrial lead were placed successfully and the pacemaker was successfully implanted into the left infraclavicular subcutaneous pocket, and an electrocardiogram taken 1 hour after surgery revealed that the pacemaker was working correctly (Figure 1D). The patient had no relevant unpleasant symptoms during the operation. Transthoracic echocardiography performed 1 hour after surgery revealed no obvious cardiac lesion or perforation. The result of pathological examination showed the tissue consisted of smooth muscle (minority) and fibrous tissue (majority) (HE staining) (Figure 1E,1F).
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was provided by the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
In cardiac pacemaker implantation, the active pacing leads and passive leads are both stable and reliable (7). The incidence of complications (lead dysfunction, perforation, dislodgement, pericarditis, pericardial effusion, tamponade, pericardiocentesis, and/or lead revision) is relatively low (8,9), and tissue-induced winding of fixation leads has never been reported.
The most likely source of the tissue remained unclear. Fixation lead implantation process may cause vascular and cardiac injuries, but the fixation leads were successfully extracted without cardiac lesion or subcutaneous hematoma, in addition, we could not determine the histological type according to the results of HE staining, which made it difficult for us to judge the source of the tissue. We can only speculate that this tissue was from musculature/soft tissue; we inserted two 7F sheaths to place the ventricular and atrial leads, and this process might have caused damage to musculature/soft tissue in the subclavian region, the musculature/soft tissue might attach to the head of the ventricular or atrial lead, which eventually led to the fixation leads winding.
Acknowledgments
Funding: This work was supported by
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://qims.amegroups.com/article/view/10.21037/qims-23-639/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was provided by the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Defaye P, Biffi M, El-Chami M, Boveda S, Glikson M, Piccini J, Vitolo M. Cardiac pacing and lead devices management: 25 years of research at EP Europace journal. Europace 2023;25:euad202. [Crossref] [PubMed]
- Glikson M, Nielsen JC, Kronborg MB, Michowitz Y, Auricchio A, Barbash IM, et al. 2021 ESC Guidelines on cardiac pacing and cardiac resynchronization therapy. Eur Heart J 2021;42:3427-520. [Crossref] [PubMed]
- Kirkfeldt RE, Johansen JB, Nohr EA, Jørgensen OD, Nielsen JC. Complications after cardiac implantable electronic device implantations: an analysis of a complete, nationwide cohort in Denmark. Eur Heart J 2014;35:1186-94. [Crossref] [PubMed]
- Ozcan KS, Osmonov D, Altay S, Dönmez C, Yıldırım E, Türkkan C, Güngör B, Ekmekçi A, Alper AT, Gürkan K, Erdinler I. Pacemaker implantation complication rates in elderly and young patients. Clin Interv Aging 2013;8:1051-4. [Crossref] [PubMed]
- Kollmann A, Demirbas S, Bley T, Petritsch B. Twiddler's syndrome as a rare cause of pacemaker dysfunction. Rofo 2023; Epub ahead of print. [Crossref] [PubMed]
- Lazaros G, Tsioufis C, Milkas A, Stefanadis C. Winding without twiddling of a pacemaker wire. Eur Heart J 2013;34:88. [Crossref] [PubMed]
- Liu L, Tang J, Peng H, Wu S, Lin C, Chen D, Zhang Q, Liang Y, Chen S, Chen Y, Wei H. A long-term, prospective, cohort study on the performance of right ventricular pacing leads: comparison of active-fixation with passive-fixation leads. Sci Rep 2015;5:7662. [Crossref] [PubMed]
- Palmisano P, Facchin D, Ziacchi M, Nigro G, Nicosia A, Bongiorni MG, Tomasi L, Rossi A, De Filippo P, Sgarito G, Verlato R, Di Silvestro M, Iacopino S. Rate and nature of complications with leadless transcatheter pacemakers compared with transvenous pacemakers: results from an Italian multicentre large population analysis. Europace 2023;25:112-20. [Crossref] [PubMed]
- Lowe M, Nguyen L, Patel DJ. A Review of the Recent Advances of Cardiac Pacemaker Technology in Handling Complications. J Long Term Eff Med Implants 2023;33:21-9. [Crossref] [PubMed]


