
A case of multiple Rasmussen’s aneurysm
Introduction
Rasmussen’s aneurysm is an inflammatory pseudoaneurysm of the pulmonary artery secondary to pulmonary tuberculosis, with a prevalence of 7 per 100,000 (1,2). Pathologically, the adventitia and media of the pulmonary artery wall are gradually weakened, eventually leading to the formation of a pseudoaneurysm due to the infiltration of granulation tissue (3). Hemoptysis is the most common and significant symptom, and early endovascular embolization is recommended to prevent potentially fatal hemoptysis (4-6). Herein, we report an extremely rare case of multiple Rasmussen’s aneurysm.
Case presentation
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Declaration of Helsinki (as revised in 2013). Written informed consent was provided by the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
A 59-year-old man presented to our hospital with a 2-month history of cough and expectoration, and two episodes of hemoptysis within the recent 10 days. He had a medical history of pulmonary tuberculosis and was currently receiving anti-tuberculosis treatment. A physical examination revealed rale and diminished breath sounds over the left lung, and blood routine examination presented an elevated white blood cell count of 17.7×109/L.
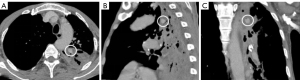
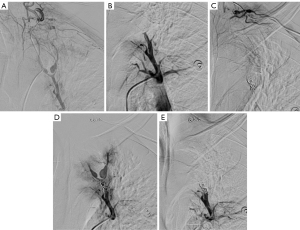
The chest contrast-enhanced computed tomography (CT) [window setting: level, 40; width, 400 Hounsfield unit (HU)] demonstrated an aneurysm with size of about 15 mm × 8 mm contained in the consolidated upper lobe of the left lung (Figure 1A-1C). Approximately 52 hours after the CT examination, non-bronchial systemic collateral artery angiography was performed and found a smaller (about 8 mm × 5 mm) aneurysm (Figure 2A). However, the initial preoperative pulmonary angiography did not find the pulmonary artery pseudoaneurysms (PAPs) due to obstructions of shunting non-bronchial systemic collateral arteries-pulmonary artery (Figure 2B). The non-bronchial systemic collateral artery originated from the thyrocervical trunk. The two adjacent aneurysms originated from the branches of the pulmonary artery. After non-bronchial systemic collateral and pulmonary artery embolization for the Rasmussen’s aneurysms (Figure 2C-2E), the patient’s symptoms were relieved.
Discussion
Rasmussen’s aneurysm is a PAP secondary to tuberculosis. The duration reported between tuberculosis diagnosis and aneurysm discovery is 6.24±6.23 months (3,7). In the duration after tuberculosis, the inflammatory granulation tissue gradually replaces the adventitia and media of the vessel wall, which is progressively weakened to form pseudoaneurysm. Hemoptysis is often the initial manifestation, and may be massive and fatal (8,9). Therefore, prompt diagnosis is necessary.
Chest contrast-enhanced CT has become the first-line diagnostic instrument for Rasmussen’s aneurysm in tuberculosis patients with recurrent hemoptysis (10-12). Multiplane reconstruction (MPR) of contrast-enhanced CT is useful in identification of aneurysm and evaluating anatomical details, which is valuable for selective angiography instruction and subsequent endovascular therapy (13,14). However, interventional angiography still has the advantage in real-time hemodynamic evaluation of the vascular bed, and some pseudoaneurysm not seen on contrast-enhanced CT may be identified by interventional angiography. Therefore, angiography should be considered as an important diagnostic tool to compensate for the pitfalls of other diagnostic modalities, especially in cases such as massive hemoptysis or multiple mild hemoptysis after bronchial artery embolization, and chronic tuberculous cavity with episodes of massive hemoptysis.
In summary, we have reported an extremely rare case of multiple Rasmussen’s aneurysm identified by contrast-enhanced CT and interventional angiography. The current case highlights the importance of interventional angiography in revealing multiple aneurysms, which are not visible on contrast-enhanced CT alone.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://qims.amegroups.com/article/view/10.21037/qims-23-460/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Declaration of Helsinki (as revised in 2013). Written informed consent was provided by the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Jadhav SS, Dhok A, Chaudhari SV, Khandaitkar S, Ambhore AN. Rasmussen's Aneurysm: A Rare Case. Cureus 2022;14:e25740. [PubMed]
- Cheng YS, Lu ZW. Bronchial aneurysm secondary to tuberculosis presenting with fatal hemoptysis: a case report and review of the literature. J Thorac Dis 2014;6:E70-2. [PubMed]
- Yi S, Wang L. Clinical features of tuberculous pseudoaneurysm and risk factors for mortality. J Vasc Surg 2022;75:1729-1738.e2. [Crossref] [PubMed]
- Zugazaga A, Stachno MA, García A, Tovar G, Benito V, Guasch I, Nogueira I, Puyalto P, Sampere J. Pulmonary artery pseudoaneurysms: endovascular management after adequate imaging diagnosis. Eur Radiol 2021;31:6480-8. [Crossref] [PubMed]
- Patankar T, Prasad S, Deshmukh H, Mukherji SK. Fatal hemoptysis caused by ruptured giant Rasmussen's aneurysm. AJR Am J Roentgenol 2000;174:262-3. [Crossref] [PubMed]
- Furuyama K, Hirama N, Fukushima S, Inage M, Ota H, Sato K, Yamauchi K, Sato M, Igarashi A, Inoue S, Watanabe M. A case of pulmonary tuberculosis with hemoptysis from a peripheral pulmonary aneurysm. EXCLI J 2021;20:1482-5. [PubMed]
- Sahoo S, Panigrahi MK, Naik S, Mohapatra PR. Rasmussen's aneurysm masquerading as mass lesion. BMJ Case Rep 2020;13:e232669. [Crossref] [PubMed]
- Jaber JF, Innabi A, Patel DC. Rasmussen's aneurysm: a rare and potentially fatal cause of hemoptysis. Am J Trop Med Hyg 2022;106:1579-80. [Crossref]
- Kawashima A, Hirose T, Horiba M. Hemoptysis from Rasmussen's Aneurysm. Am J Trop Med Hyg 2022; Epub ahead of print. [Crossref] [PubMed]
- Branco MT, Mello DFE, Ibrahim INAF, Marchiori E, Valentin MVN. Giant Rasmussen's aneurysm. J Bras Pneumol 2021;47:e20200648. [Crossref] [PubMed]
- Gallardo MEA. Giant Rasmussen's aneurysm in a 9-year-old boy: A case report. Radiol Case Rep 2022;17:4168-75. [Crossref] [PubMed]
- Garcia-Reina S, Martinez-Barenys C, Fernandez E. Giant Rasmussen's Aneurysm. Ann Thorac Surg 2018;106:e205. [Crossref] [PubMed]
- Chen Y, Gilman MD, Humphrey KL, Salazar GM, Sharma A, Muniappan A, Shepard JO, Wu CC. Pulmonary Artery Pseudoaneurysms: Clinical Features and CT Findings. AJR Am J Roentgenol 2017;208:84-91. [Crossref] [PubMed]
- Arif A, Bhinder KK, Sarfraz A, Sarfraz Z, Felix M, Chérrez-Ojeda I. The radiological presentation of Rasmussen aneurysm secondary to pulmonary tuberculosis and COVID-19: A case report. Radiol Case Rep 2021;16:3350-3. [Crossref] [PubMed]


