
Isotropic dynamic contrast-enhanced magnetic resonance imaging using differential subsampling with cartesian ordering and adaptive imaging receive coil for the diagnosis of Crohn disease: a case description
Introduction
Crohn disease (CD) is a chronic inflammatory bowel disease that primarily affects young people and is increasing in incidence worldwide, particularly in Asia (1). The symptoms are diarrhea, abdominal pain, fatigue, and weight loss, with recurrence and remission being common (2). The underlying cause of CD is unknown; however, it is clear that both environmental and genetic factors are required for its development. Magnetic resonance enterography (MRE) is a noninvasive technique that can assess the extent and activity of disease based on wall thickness and significant contrast enhancement without radiation exposure. Due to the limitation of slice thickness and signal-to-noise ratio (SNR), ordinary magnetic resonance imaging (MRI) cannot perform high-resolution isotropic imaging. New adaptive imaging receive (AIR) coil is made up of a fiber guide ring structure instead of common copper circuit, facilitating ultra-high density coil unit channel distribution (3). The use of an AIR coil significantly improves the SNR of images and enables isotropic imaging, which reduces the partial volume effect and provides a comprehensive view of the inside and outside of the intestine from any aspect. Liver acquisition with volume acceleration (LAVA) is widely used in clinical abdominal imaging, but requires a compromise between high temporal and spatial resolution. Therefore, the conventional LAVA sequence cannot achieve isotropic dynamic-enhanced scanning. Differential subsampling with cartesian ordering (DISCO) combines a dual-echo spoiled gradient-recalled (SPGR) sequence with pseudo-random variable density k-space segmentation and a view sharing reconstruction, allowing for the collection of 3D volumes with an improved temporal resolution of 15 seconds while maintaining robust spatial resolution and image quality, thus providing dynamic contrast-enhanced MRI (DCE-MRI) (4). DCE-MRI is a functional imaging method that exploits vessel density, integrity, and permeability (5). A prospective study demonstrated that DCE-MRI was a promising technique for the assessment of severity and activity of CD using pharmacokinetic parameters (6). The case described here represents the first use of isotropic DCE-MRI examination with AIR coil and the DISCO technique to enhance CD diagnosis.
Case presentation
A 15-year-old female patient complained of diarrhea occurring over the previous 6 months. She also had associated weight loss (13.5 kg), intermittent oral ulcerations, mucopurulent bloody stool, and fever (up to 39.9 ℃). She was nonsmoker and had no family history of inflammatory bowel disease or cancer.
On examination, she was dehydrated and had no fever. Her pulse rate was 120 beats per minute, her blood pressure was 85/56 mmHg, and her respiratory rate was 20 cycles per minute.
Abdominal examination showed deep tenderness in the lower right quadrant, with no rebound pain, palpable mass, or draining fistula.
Investigations
Blood examination showed a reduced hemoglobin level (102 g/L), red cell count (3.52×1012/L), leukocyte count (3.61×109/L), and albumin level (30.4 g/L); an elevated platelet count (433×109/µL), erythrocyte sedimentation rate (69 mm/h), C-reactive protein level (109 mg/L), and procalcitonin level (0.16 ng/mL); and normal tuberculosis antibody status. The fecal occult blood test was positive.
To check for intestinal parasite infection, microbiological examinations were performed, including blood cultures, serologies for viruses (hepatitis B virus, hepatitis C virus, tuberculosis, HIV), immunoglobulins (toxoplasma, rubella virus, cytomegalo virus, herpes simplex virus, immunoglobin M, antineutrophil cytoplasmic antibodies, extractable nuclear antigen, antinuclear antibody), tuberculosis-interferon-gamma release assays, and quantification of DNA (Epstein-Barr virus, cytomegalovirus), yielding normal findings.
With the above-described symptoms being the focus, the patient underwent isotropic DCE-MRI examination with DISCO protocols and AIR coil, after an intravenous bolus of 0.2 mmol·kg−1 body weight of gadopentetate dimeglumine was administered into an arm vein at a rate of 3 mL/s. DISCO contained 20 dynamic phases and was acquired with a respiratory navigator. The imaging parameters for DISCO were as follows: repetition time/time to echo (TR/TE) 2.9 ms/1.0 ms, flip angle 12°, field of view 40 mm × 30 mm, spatial resolution 1.6 mm × 1.6 mm × 1.6 mm, and temporal resolution 15.6 s. LAVA was acquired with a breath hold after DISCO. Imaging parameters for LAVA were as follows: TR/TE 3.5 ms/1.5 ms, flip angle 15°, field of view 48 mm × 38.4 mm, spatial resolution 1.6 mm × 1.6 mm × 1.6 mm, and total scan time 22 s. Diffusion-weighted imaging (DWI) was also performed. The imaging parameters for DWI were as follows: field of view 380 mm × 323 mm, slice thickness 4 mm, space 0 mm, matrix 128×128, scan time 182 s, and b values 10, 20, 50, 100, 150, 200, 400, 600, and 800. MR images clearly revealed widely uneven wall thickening of the terminal ileum, ileocecal valve, ascending colon, transverse colon, and sigmoid colon inferior segment, with asymmetric mural hyperenhancement and restricted diffusion of water molecules, mesenteric fat infiltration with increased mesenteric vascularity (“comb” sign), and enlarged mesenteric lymph nodes with remarked enhancement, which are all highly indicative of CD (Figure 1). Postprocessing were performed on Gen IQ (GE Healthcare) using the standard Tofts model and a 2-parameter fitting algorithm to obtain pharmacokinetic quantitative data including transfer constant (Ktrans), efflux rate (Kep), extravascular extracellular volume (Ve) (Figure 2; Table 1).
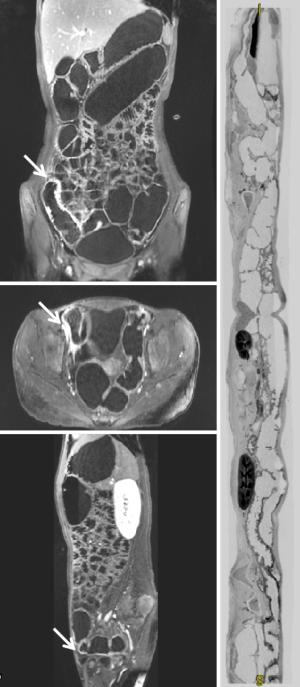
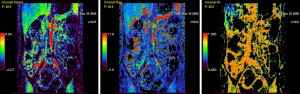
Table 1
| Parameter | Terminal ileum | Ileocecal junction | Ascending colon | Transverse colon | Descending colon | Sigmoid colon |
|---|---|---|---|---|---|---|
| Ktrans (min−1) | 1.72±0.82 | 0.91±0.13 | 0.92±0.12 | 0.59±0.08 | 0.21±0.09 | 0.71±0.23 |
| Kep (min−1) | 2.58±2.07 | 1.51±0.30 | 3.61±1.34 | 2.86±1.01 | 0.93±0.39 | 1.61±0.97 |
| Ve | 0.88±0.02 | 0.68±0.15 | 0.34±0.12 | 0.21±0.11 | 0.29±0.07 | 0.64±0.28 |
Data are presented as mean ± standard deviation.
Ileo-colonoscopy revealed a 0.3 cm sessile polypoid mass 10 cm away from the anal verge. Numerous ulcerative, hemorrhagic, and polypoid lesions were found in the area spanning from the terminal ileum to the whole colon, except for the descending colon. The lesions were discontinuous and longitudinal, with the regular intestine tissues between the lesions and ulcers characterized by a “cobblestone” appearance in the ascending colon (Figure 3).
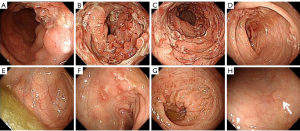
The polypoid mass, ileocecal valve, and the colonic and ileal mucosa were biopsied. The biopsies of rectal polyps showed granulation tissue proliferation with inflammatory cell infiltration. The biopsies of the colonic and ileal mucosa showed chronic mucosal inflammation with eosinophilic infiltration, formation of lymphoid follicles, and granulation tissue proliferation.
Multidisciplinary team (MDT) discussions confirmed the diagnosis of CD based on the clinical manifestations and examinations described above. The patient had no indications for surgery and was treated with the injection of biologics Remicade (infliximab, 200 mg) intravenously, Enteral Nutritional Powder (TP, 55.8 g) 4 times a day, and anti-infective therapy with metronidazole (0.4 g) twice a day, which achieved significant therapeutic effect without any side effects. The patient received the same treatment 2 weeks later.
All procedures performed in this study were in accordance with the ethical standards of the institutional ethics committee of Sichuan University West China Hospital and with the Declaration of Helsinki (as revised in 2013). Written informed consent was obtained from the patient’s parent for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
Common MRE protocols typically consist of T2-weighted imaging (with and without fat suppression), balanced steady-state free precession gradient-echo (b-SSFP) sequences, gradient-echo (GRE) sequences, and fast spin echo techniques (7). GE Healthcare, Philips, and Siemens might have differences in the naming of these sequences. In recent years, newly suggested scan protocols (in addition to LAVA) have also been proposed for improving MRE image quality. Sensitivity encoding (SENSE) and compressed sensing–SENSE (CS-SENSE) protocols could provide shorter scan times with reduced artifacts and improved image quality in MRE, which contribute to a better diagnostic performance related to CD (8). MRE performed with DWI sequences (diffusion factor b fixed at 50, 400, and 800 s/mm2) has been found to be comparable to T1-weighted postcontrast sequences, especially for inflammatory bowel disease (9). DCE-MRE performed with T1-weighted high resolution isotropic volume examination (THRIVE) sequences offer the following quantitative perfusion parameters: relative arterial (RAE), venous (RVE), and late enhancement (RLE); maximum enhancement (ME); and time to peak (TTP). These have been reported to be helpful in differentiating inflamed from fibrotic bowel wall vascularity (10). MR-fluoroscopic sequences have also been used to assess bowel distension or stricture (11). b-SSFP was also recently proposed as an MRE protocol for CD activity and complication assessment and has shown robust agreement with the full MRE protocol (12).
This case report is the first to evaluate the image performance of a new MRE protocol known as isotropic DCE-MRI using DISCO and AIR coil techniques from a subjective perspective. The images clearly showed the location, morphology, size, and relationship to adjacent tissues of the lesion with fewer artifacts and significantly improved scanning speed. Moreover, it performed isotropic thin-slice scanning while preserving high spatiotemporal resolution and demonstrated higher Ktrans values of bowel lesions than of normal tissue.
Given its ability to examine disease extent, activity, severity, and mural and extramural complications, as well as curative effect, prevention, and surveillance, MRE is gaining increasing importance in the evaluation of the intestinal tract, especially in patients with CD (13). Hafeez et al. found that MRE could increase clinician's diagnostic confidence and influence therapeutic strategy in 61% of the patients with CD (14).
However, there are still some challenges related to MRE: (I) it has a long scan time, (II) early lesions are not clinically identifiable, and (III) the proximal small intestine is poorly dilated (15). A study evaluating the impact of AIR coil in brain MRI imaging confirmed that AIR coil significantly increased the SNR level (3). Isotropic imaging can be realized on the basis of the improved SNR level of the image, which is helpful for finding early lesions and identifying intestinal peristalsis artifacts through providing a comprehensive view of the inside and outside of the intestine from any aspect. As the LAVA sequence requires k-space full sampling, the temporal resolution of LAVA is 20–30 s with the adequate spatial resolution. DISCO samples an elliptically ordered central k-space region each time, subsamples the outer regions with pseudo-random segmentation, and can achieve a time resolution of 15.6 s without compromising temporal or spatial resolution, thus making DCE-MRI examination feasible. The combination of AIR coil and DISCO technology is expected to further improve image quality and diagnostic efficiency.
We should, however, be aware of a few limitations. Insufficient DISCO sampling may lose image details, making it necessary to balance temporal and spatial resolution. Moreover, spasms will cause incorrect pharmacokinetic parameters, which can be improved by administering an anticholinergic drug before scanning. Furthermore, the multiphase images should be reviewed and images with large peristalsis deleted. Finally, due to the adoption of navigator respiratory monitoring, even diaphragm motility is required during the examination.
Conclusions
This report presents a novel diagnostic method of CD using the DISCO technique with AIR coil. Isotropic DCE-MRI can dramatically improve temporal resolution so as to provide detailed morphological and functional information for the diagnosis of CD. Patients with CD or other gastrointestinal disorders can be expected to benefit from isotropic DCE-MRI examination.
Acknowledgments
Funding: This work was partially supported by the Sichuan Province Science and Technology Support Program (grant No. 2021YJ0241).
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://qims.amegroups.com/article/view/10.21037/qims-22-1256/coif). HY, LN, and BZ are employees of GE Healthcare. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional ethics committee of Sichuan University West China Hospital and with the Declaration of Helsinki (as revised in 2013). Written informed consent was obtained from the patient’s parent for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Ng SC, Tang W, Ching JY, Wong M, Chow CM, Hui AJ, et al. Incidence and phenotype of inflammatory bowel disease based on results from the Asia-pacific Crohn's and colitis epidemiology study. Gastroenterology 2013;145:158-165.e2. [Crossref] [PubMed]
- Torres J, Mehandru S, Colombel JF, Peyrin-Biroulet L. Crohn's disease. Lancet 2017;389:1741-55. [Crossref] [PubMed]
- Cogswell PM, Trzasko JD, Gray EM, Campeau NG, Rossman PJ, Kang D, Robb F, Stormont RS, Lindsay SA, Bernstein MA, McGee KP, Huston J 3rd. Application of Adaptive Image Receive Coil Technology for Whole-Brain Imaging. AJR Am J Roentgenol 2021;216:552-9. [Crossref] [PubMed]
- Saranathan M, Rettmann DW, Hargreaves BA, Clarke SE, Vasanawala SS. DIfferential Subsampling with Cartesian Ordering (DISCO): a high spatio-temporal resolution Dixon imaging sequence for multiphasic contrast enhanced abdominal imaging. J Magn Reson Imaging 2012;35:1484-92. [Crossref] [PubMed]
- Boss MK, Muradyan N, Thrall DE. DCE-MRI: a review and applications in veterinary oncology. Vet Comp Oncol 2013;11:87-100. [Crossref] [PubMed]
- Hectors SJ, Gordic S, Semaan S, Bane O, Hirten R, Jia X, Colombel JF, Taouli B. Diffusion and perfusion MRI quantification in ileal Crohn's disease. Eur Radiol 2019;29:993-1002. [Crossref] [PubMed]
- Maccioni F, Bruni A, Viscido A, Colaiacomo MC, Cocco A, Montesani C, Caprilli R, Marini M. MR imaging in patients with Crohn disease: value of T2- versus T1-weighted gadolinium-enhanced MR sequences with use of an oral superparamagnetic contrast agent. Radiology 2006;238:517-30. [Crossref] [PubMed]
- Kim J, Seo N, Bae H, Kang EA, Kim E, Chung YE, Lim JS, Kim MJ. Comparison of Sensitivity Encoding (SENSE) and Compressed Sensing-SENSE for Contrast-Enhanced T1-Weighted Imaging in Patients With Crohn Disease Undergoing MR Enterography. AJR Am J Roentgenol 2022;218:678-86. [Crossref] [PubMed]
- Masselli G, De Vincentiis C, Aloi M, Guida M, Cao R, Cartocci G, Miele V, Grassi R. Detection of Crohn's disease with diffusion images versus contrast-enhanced images in pediatric using MR enterography with histopathological correlation. Radiol Med 2019;124:1306-14. [Crossref] [PubMed]
- Ippolito D, Lombardi S, Talei Franzesi C, Drago SG, Querques G, Casiraghi A, Pecorelli A, Riva L, Sironi S. Dynamic Contrast-Enhanced MR with Quantitative Perfusion Analysis of Small Bowel in Vascular Assessment between Inflammatory and Fibrotic Lesions in Crohn's Disease: A Feasibility Study. Contrast Media Mol Imaging 2019;2019:1767620. [Crossref] [PubMed]
- Cicero G, D'Angelo T, Bottari A, Costantino G, Visalli C, Racchiusa S, Marino MA, Cavallaro M, Frosina L, Blandino A, Mazziotti S. Superior Mesenteric Artery Syndrome in Patients with Crohn's Disease: A Description of 2 Cases Studied with a Novel Magnetic Resonance Enterography (MRE) Procedure. Am J Case Rep 2018;19:431-7. [Crossref] [PubMed]
- Jhaveri KS, Sagheb S, Guimaraes L, Krishna S, Ahari AF, Espin-Garcia O. Evaluation of Crohn Disease Activity Using a Potential Abbreviated MRE Protocol Consisting of Balanced Steady-State Free Precession MRI Only Versus Full-Protocol MRE. AJR Am J Roentgenol 2021;216:384-92. [Crossref] [PubMed]
- Maaser C, Sturm A, Vavricka SR, Kucharzik T, Fiorino G, Annese V, et al. ECCO-ESGAR Guideline for Diagnostic Assessment in IBD Part 1: Initial diagnosis, monitoring of known IBD, detection of complications. J Crohns Colitis 2019;13:144-64. [Crossref] [PubMed]
- Hafeez R, Punwani S, Boulos P, Bloom S, McCartney S, Halligan S, Taylor SA. Diagnostic and therapeutic impact of MR enterography in Crohn's disease. Clin Radiol 2011;66:1148-58. [Crossref] [PubMed]
- Griffin N, Grant LA, Anderson S, Irving P, Sanderson J. Small bowel MR enterography: problem solving in Crohn's disease. Insights Imaging 2012;3:251-63. [Crossref] [PubMed]


