
The optimal tibial tunnel placement to maximize the graft bending angle in the transtibial posterior cruciate ligament reconstruction: a quantitative assessment in three-dimensional computed tomography model
Introduction
In recent decades, transtibial posterior cruciate ligament (PCL) reconstruction has evolved as a common surgical technique to restore the stability of the knee joint after the PCL laceration (1,2). However, the transtibial technique is also considered to be one of the important reasons for postoperative PCL graft abrasion and elongation because an acute graft bending angle (GBA) called “killer turn” is unavoidably created at the proximal tibial tunnel aperture (3,4). Several studies have suggested that a sharper “killer turn” is correlated with a higher shear stress concentrated on the PCL graft (5-7). As previous studies reported, different tibial tunnel placements may change the GBA, thus affecting the killer turn effect (5,8).
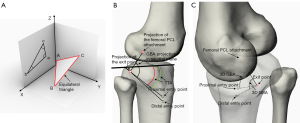
Clinically, increasing the tibial tunnel angle (TTA) in anteromedial approach is a traditional method to reduce the killer turn effect (8-10). The formation of this view is largely because the surgeons could observe an increased GBA on the sagittal plane of the computed tomography (CT) or magnetic resonance imaging (MRI) after increasing the TTA (11). Therefore, it is a common belief that a greater TTA means a greater GBA, and many studies have been to explore how to maximize the TTA (10,12). However, the GBA is an angle in the three-dimensional (3D) space, while the GBA viewed on the CT or MRI is just a projection angle. From a mathematical point of view, the 3D angle between two vectors is not determined by the 2-dimensional (2D) angles between their projections into a coordinate plane (13). For example, Figure 1A shows that the three angles of an equilateral triangle in 3D space remain the same when its projection angle is varied. Therefore, increasing the TTA may just cause a greater projection angle of the GBA in sagittal plane, but not the real 3D GBA (Figure 1B,1C have shown that the variation of the 3D GBA is unclear when the TTA increased, but the projection of the GBA is increased). Most importantly, few studies have proved that the clinical practice of increasing the TTA is a correct method that leads to an increase in 3D GBA. Therefore, there should be more theoretical studies to explore the relationship between the tibial tunnel placement and the GBA.
When performing the transtibial PCL reconstruction using the anteromedial tibial tunnel approach, it is easier to place the sleeve of the drill guide over the tibial cortex, and is easier to drill and ream (14). While the recommendation of the anterolateral approach is largely because it provides a greater GBA (5,7). However, a recent study of Teng et al. (10) has shown that the maximum possible angle of the tibial tunnel relative to the tibial plateau is 58° in anteromedial approach, 50° in anterolateral approach. Therefore, the TTA could be increased greater when using the anteromedial approach to perform the PCL reconstruction. However, few studies have revealed how the TTA affects the GBA, and have further compared the effect of increasing TTA on GBA and changing anteromedial approach to anterolateral approach on GBA (10). This information is very important for surgeons to determine how to place the tibial tunnel, and for ensuring the optimal tibial tunnel to reduce the killer turn effect. To date, the optimal tibial tunnel placement to maximize the GBA remains unclearly.
In present study, the purposes were to (I) provide a method to quantitively analyze the GBA based on the 3D CT, and discuss the optimal tibial tunnel placement to minimize the killer turn effect in the transtibial PCL reconstruction; (II) reveal how the GBA varied as the tibial tunnel entrance changed from proximal to distal.
Methods
Sample selection
This was an in-vitro 3D computer simulation study. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The Ethics Committee of Lanzhou University Second Hospital approved this study (No. 2021A-169), and the requirement to obtain individual consent for this retrospective analysis was waived. Patients with knee injuries who took CT scanning were selected from the CT database (April 2020 to January 2022) in local hospital for review. The following CT images were considered to include in this study: (I) Kellgren-Lawrence grade of knee osteoarthritis was less than 1; (II) the tibial PCL attachment could be clearly identified; (III) the resolution was ultrahigh; (IV) patients aged from 18 to 60. The CT images showed fractures, knee surgery history, injuries on soft tissues and morphological abnormalities were excluded. At last, 55 CT images were selected based on the inclusion and exclusion criteria. The patient demographic data were shown in Table 1.
Table 1
| Parameter | Value |
|---|---|
| Number | 55 |
| Sex (male/female) | 27:28 |
| Age (year) | 33.9±7.8 [18–47] |
| Height (m) | 1.66±0.09 [1.44–1.90] |
| BMI (kg/m2) | 23.7±3.9 [15.9–32.9] |
Date are presented as n or mean ± SD [range].
Computational procedures
CT images were obtained from a 64-multi-detector-row CT scanner (Siemens AG, Wittelsbacherplatz 2, Muenchen, Germany) using a supine position. We used the following parameters for CT images: a gantry rotation speed of 1.00 s/rotation, 0.625 mm collimation width ×12 detectors, a CT pitch factor of 0.90, and a field of view of 25 to 30 cm. The CT images were saved as Digital Imaging and Communications in Medicine (DICOM) format, which were processed by MIMICS software (Materialise, Leuven, Belgium) to create 3D knee model. The created knee models were imported to the Rhinoceros 3D modeling software (Rhino 7, Robert McNeel and Associates for Windows, Washington DC, USA) to simulate the PCL reconstruction and proceed the measurement.
Femoral PCL attachments on the 3D knee model
Previous study of Johannsen et al. (15) have shown, the PCL’s anterolateral bundle (ALB) and posteromedial bundle (PMB) center on the lateral view were respectively located 14.1 and 15.8 mm superior to the distal condyle line (the distal margins of the femoral condyle), and respectively located 4.7 and 10.7 mm posteroinferior from the Blumensaat line) (15). In order to simplify the measurement, the midpoint of the ALB and PMB on the medial femoral condyle was defined as the PCL attachment center. In present study, to obtain the true lateral view of the femur, the 3D knee model was adjusted on the Rhinoceros 3D modeling software to strictly overlap the medial and lateral femoral condyles (10,16). The transparency of the knee model was adjusted to emerging the Blumensaat’s line on the lateral view (Figure 2A). Then the PCL attachment projection (7.7 mm posteroinferior to the Blumensaat’s line and 15 mm superior to the distal condyle line) could be marked by a point on the lateral view (Figure 2A). Using the projection function of the Rhinoceros software to project the point on the femoral medial condyle, then the real femoral PCL attachment point was obtained in 3D view (Figure 2B).
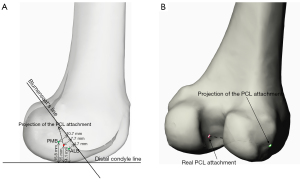
Tibial PCL attachments on the 3D knee model
As previous studies described, after manually adjusting the grayscale value of the CT image, the widest and clearest PCL attachment could be observed on the sagittal section (10,11). A point was marked on the center of the tibial PCL footprint, and the 3D coordinate of the point was recorded on the Mimics software. This 3D coordinate was input into the Rhinoceros 3D modeling, then the center point of the tibial PCL attachment was acquired (Figure 3).
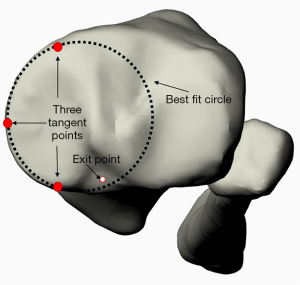
Entry points of the tibial tunnels
When simulating the tibial tunnels, the tibial PCL attachment was defined as the exit point, the medial tibial plateau plane was defined as the reference plane. A best fit circle was manually created tangent to the cortical edge of medial tibial plateau (17). Then three tangent points could be marked between the circle and the medial tibial plateau (12) (the peak point of the anterior side of the medial tibial plateau; the most medial point of the tibial plateau; the peak point of the posterior side of the medial tibial plateau). The three points were connected to generate the tibial plateau plane (Figure 3).
In clinical practice, the tibial guide system was commonly placed at an angle from 45° to 55°. A previous study has reported, the maximum angle between the tibial tunnel and tibial plateau was 58° for anteromedial approach, and was 50° for anterolateral approach (10). Therefore, the tibial tunnel at an angle of 40°, 50° and 60° relative to the tibial plateau were simulated on anteromedial and anterolateral tibia in present study. The detailed methods to locate the tibial tunnel entrance was shown as follows. Firstly, three tibial tunnel lines, which were 40°, 50° and 60°related to the medial tibial plateau plane and passed the exit point of tibial tunnel, were drawn in 3D view (Figure 4A). Secondly, the entry points of the tibial tunnels were placed at 2 cm posterolateral and posteromedial from the most anterior position of the tibial crest (Figure 4B,4C). The connecting line of the entry point and the center point of the tibial PCL attachment was defined as the center line of the tibial tunnel (Figure 4B).
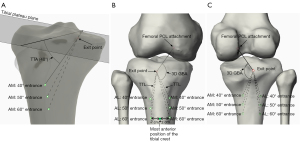
Outcome measurements
The GBA and the tibial tunnel length (TTL) were measured in this study. GBA was the angle between the graft inside tibial tunnel and the graft inside knee joint. Therefore, in present study, the GBA could be defined as the angle of the center line of the tibial tunnel relative to the connecting line of the center point of the tibial and femoral PCL attachment. The TTL was defined as the distance between the entry point and exit point of the tibial tunnel (Figure 4B,4C). The TTA was defined as the angle between the center line of the tibial tunnel and the tibial plateau plane. The measurement was undertaken by two board-certified orthopedic surgeons, who received standard training for simulating the transtibial PCL reconstruction on the 3D modeling software. The intra-observer reproducibility was ensured by one surgeon measuring the required data two times at least 4 weeks apart. The inter-observer reproducibility was ensured by another surgeon who performed the same measurement procedure. The intraclass correlation coefficients (ICCs) was used to evaluate the intra-observer and inter-observer reproducibility. ICC >0.75 was considered excellent agreement (18,19). Regarding the GBA, intra-observer ICC and inter-observer ICC values were 0.909 and 0.894 respectively, which indicate a high consistency of measurements within an observer and between the observers.
Statistical analysis
The F test function of the G*Power software (version 3.1.9, Heinrich Heine University, Düsseldorf, Germany) was used to calculate the minimum sample size (ANOVA: Repeated measures; A priori) (effect size =0.62; 1-β err prob =0.9; α =0.05) based on the pre-experiment data of different GBA in 40°, 50° and 60° TTA groups. All the data were processed by the SPSS software (version 26.0, Inc., Chicago, IL, USA). Mean ± standard deviation was used to express the result. A repeated measures ANOVA was used to compare differences among 40°, 50° and 60° TTA groups, P<0.05 was considered statistically significant. The Kolmogorov-Smirnov test was used to evaluate whether the data obeyed the normal distribution. Independent t-test was used to compare the differences between two groups. Correlation between the GBA and TTA, patients’ anthropomorphic characteristics of age, height, and BMI were evaluated by Pearson’s (used for two normally distributed variables) or Spearman’s (used for nonnormally distributed variables) correlation analysis. Correlation coefficients (r) was used to assess the correlative degree of two variables: 0.1<r<0.3 indicating weak correlation, 0.3<r<0.7 indicating moderate correlation, and 0.7<r<1.0 indicating strong correlation. The GraphPad Prism (version 9; GraphPad Software, Inc.) software was used to process the linear regression analysis to identify the effect on the GBA by the TTA, and to obtain the best-fit equations between them. Goodness of fit and predictive ability of all models was evaluated by coefficients of determination (r2).
Results
In present study, twenty CT images were used for pre-experiment, and the minimum sample size calculated was 27. Therefore, the sample size of this study was sufficient. The data of the GBA and TTL in 40°, 50° and 60° TTA groups, the height and BMI of patients had a normal distribution.
GBA and TTL in different tibial tunnel approaches
As Table 2 showed, the GBA in anterolateral approach with a 50° TTA was significantly greater than it in anteromedial approach with a 60° TTA (P<0.001). There was no difference of the GBA between the anterolateral approach with a 40° TTA and the anteromedial approach with a 60° TTA (P>0.05). The GBA in anterolateral approach was about 14.27° to 16.56° greater than in anteromedial approach (P<0.001). In anteromedial and anterolateral approaches, the GBA was increased as the TTA increased (P<0.001) (Figure 5).
Table 2
| Parameter | GBA (°) | TTL (mm) | |||
|---|---|---|---|---|---|
| AM | AL | AM | AL | ||
| TTA | |||||
| 40° | 94.68±6.6 | 111.14±6.71ab | 54.56±4.79 | 52.28±5.13abc | |
| 50° | 103.73±6.61 | 119.99±6.68abc | 62.01±5.48 | 58.99±5.66abc | |
| 60° | 112.51±6.51 | 126.78±6.59abc | 74.16±6.95 | 71.06±6.96abc | |
| P value | <0.001 | <0.001 | <0.001 | <0.001 | |
Data are presented as mean standard ± deviation. P value: comparation between 40°, 50° and 60° groups; compared with 40° TTA in AM group: a, P<0.05; compared with 50° TTA in AM group: b, P<0.05; compared with 60° TTA in AM group: c, P<0.05. GBA, graft bending angle; TTL, tibial tunnel length; AM, anteromedial approach; AL, anterolateral approach; TTA, tibial tunnel angle.
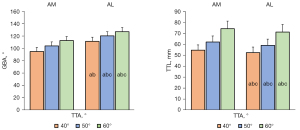
In 40°, 50° and 60° TTA groups, TTL in anteromedial tibial tunnel approach was longer than in anterolateral approach (P<0.001). In anteromedial and anterolateral approaches, the TTL was increased as the TTA increased. The TTL in anterolateral approach with a 50° TTA was significantly shorter than it in anteromedial approach with a 60° TTA (P<0.001). The TTL in anteromedial approach with a 60° TTA was about 21.88 mm longer than it in anterolateral approach with a 40° TTA (P<0.001) (Figure 5).
GBA between different sexes
In AM and AL tibial tunnel approaches, there was no difference of the GBA between sexes (Table 3).
Table 3
| Parameter | AM | AL | |||||
|---|---|---|---|---|---|---|---|
| Male (n=27) | Female (n=28) | P value | Male (n=27) | Female (n=28) | P value | ||
| TTA | |||||||
| 40° | 95.53±6.69 | 93.86±6.52 | 0.352 | 109.43±6.7 | 112.79±6.41 | 0.063 | |
| 50° | 104.55±6.72 | 102.94±6.52 | 0.373 | 118.46±6.58 | 121.46±6.55 | 0.096 | |
| 60° | 113.17±6.54 | 111.88±6.53 | 0.469 | 126.03±6.61 | 127.61±6.6 | 0.411 | |
Data are presented as mean standard ± deviation. P value: male group compared with the female group. GBA, graft bending angle; AM, anteromedial approach; AL, anterolateral approach; TTA, tibial tunnel angle.
Correlation analysis
The GBA showed a strong correlation with the TTA (for anteromedial: r=0.759, P<0.001; for anterolateral: r=0.702, P<0.001). The patient’s anthropomorphic characteristics difference of age, height and BMI were found not affect the GBA (Table 4).
Table 4
| Parameter | Height vs. GBA | Age vs. GBA | BMI vs. GBA | |||||
|---|---|---|---|---|---|---|---|---|
| r value | P value | r value | P value | r value | P value | |||
| TTA | ||||||||
| 40° (AM) | 0.019 | 0.891 | 0.074 | 0.593 | −0.154 | 0.262 | ||
| 50° (AM) | 0.008 | 0.952 | 0.057 | 0.678 | −0.173 | 0.206 | ||
| 60° (AM) | 0.01 | 0.942 | 0.040 | 0.775 | −0.166 | 0.227 | ||
| 40° (AL) | −0.327 | 0.015 | 0.342 | 0.011 | −0.047 | 0.736 | ||
| 50° (AL) | −0.305 | 0.024 | 0.248 | 0.068 | −0.072 | 0.601 | ||
| 60° (AL) | −0.222 | 0.104 | 0.165 | 0.229 | −0.124 | 0.369 | ||
BMI, body mass index; GBA, graft bending angle; AM, anteromedial approach; AL, anterolateral approach; TTA, tibial tunnel angle.
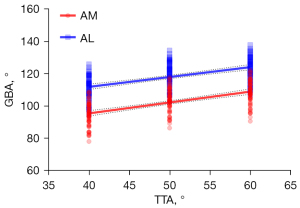
Linear regression analysis
As Figure 6 showed, in anteromedial and anterolateral approaches, the TTA has a significant proportional relationship with the GBA. The best-fit equation to calculate the GBA based on the TTA was Y = 0.89*X + 59.05 in AM tibial tunnel approach (r2=0.576), and was Y = 0.78*X + 80.21 AL tibial tunnel approach (r2=0.493). Every 10° change of the TTA caused 8.9° change of the GBA for anteromedial approach, and caused 7.8° change of the GBA for anterolateral approach.
Discussion
In present study, every 10° increase of the TTA is found to cause the GBA to increase about 8.9° for anteromedial approach, and 7.8° for anterolateral approach. Compared with maximizing the TTA in anteromedial approach (58°), maximizing it in anterolateral approach (50°) could provide a greater GBA and a shorter TTL during performing the PCL reconstruction. Besides, using the 40° TTA in anterolateral approach provides a non-differential GBA and a shorter TTL compared with maximizing the TTA in anteromedial approach (58°). Therefore, no matter how the TTA is changed in the anteromedial approach, using anterolateral approach is likely to reduce the killer turn effect more effectively than using anteromedial approach.
Does the GBA really increase as the TTA becomes greater?
Making the tibial tunnel originating from the anteromedial tibial cortex is a traditional surgical approach to the transtibial PCL reconstruction (1,14,20). However, it is also considered to cause a sharp bending angle of the graft at the proximal tibial tunnel margin (1,21,22). The angle is called “killer turn” and is regarded as an important reason for the graft abrasion (2,23,24). Several studies have revealed that the higher graft compressive force on the graft caused severer killer turn effect (5,7). Huang et al. (5) have previously built a mathematic model to explore the relationship between the compressive force on the graft and the GBA, which found that a sharper GBA is correlated with a higher graft compressive force [F = 2 × T × cos(θ/2), F: compression force; T: graft tension; θ: GBA]. Clinically, the GBA is commonly evaluated by the angle that forms by the projection of the intra-tunnel graft and the intra-articular graft on the sagittal plane (using CT or MRI). Surgeons prefer to place the tibial tunnel entrance more distal to enlarge this projection angle to reduce the killer turn effect (8). Based on this clinical preference, several studies have been to determine the maximum TTA in their study (8,10,12). However, this may be a misconception of the surgeons and the researchers about the killer turn. The GBA is an angle in 3D space. Theoretically, the 3D angle between two vectors is not determined by the 2D angles between their projections into the various coordinate planes (Figure 1) (13). Therefore, placing the tibial tunnel entrance more distal might just increase GBA’s projection angle on sagittal plane, but not the GBA. To date, few studies have analyzed the effect of the proximal-distal placement of the tibial tunnel on the GBA, and few clinical or biomechanical studies have proved that a greater TTA could reduce the killer turn effect. This study has proved that a greater TTA is correlated with a greater GBA, which could be a theoretical support for the previous clinical practice to increase the TTA during the PCL reconstruction and for the rationality of previous studying how to maximize the TTA.
The optimal tibial tunnel placement to maximize the GBA
When studying the maximum angle of tibial tunnel relative to the tibial plateau, Teng et al. (10) have found that the entrance of the anteromedial tibial tunnel could be placed more distal than of the anterolateral tunnel. Therefore, they have inferred that maximizing the TTA in the anteromedial approach may reduce killer turn effect more obviously than in the anterolateral approach. Nevertheless, their study has yet analyzed the GBA, and the effect of changing the tibial tunnel approach from anteromedial to anterolateral on the graft bending angle is neglected. Several studies have revealed that the GBA is increased as the tibial tunnel approach changes from anteromedial to anterolateral (5,7,14). However, it is unclearly whether the effect of the TTA on the GBA is greater than changing the tibial tunnel approach from anteromedial to anterolateral. Consequently, the inference of Teng et al. needs to be further proved.
According to previous studies in transtibial PCL reconstruction, recommendations for the drill guide angle have varied from 42° to 58° in anteromedial approach, and the maximum angle of the drill guide is 50° in anterolateral approach (10,25-27). In present study, the conclusion is completely contrary to the inference of Teng et al. (10). The most distal tibial tunnel in anteromedial approach has no advantage for reducing the killer turning effect, even compared with the most proximal tibial tunnel in anterolateral approach. The maximum TTA in anterolateral tibial tunnel approach is approximately about 10° less than in anteromedial approach. However, every 10° change of TTA only caused 8.9° change of GBA in anteromedial approach, while changing tibial tunnel approach from anteromedial to anterolateral could increase the GBA at least about 14.27°. Therefore, the corresponding GBA of the maximum TTA in anterolateral approach is greatest, although the maximum TTA in anterolateral approach is significantly smaller than in anteromedial approach. Consequently, in order to minimize the graft compression force in PCL reconstruction, the maximum TTA (50°) in anterolateral approach should be used.
The TTL in the PCL reconstruction
As previous studies reported, the graft abrasion caused by the killer turn is not only related to the high compression force enforced on the graft by the sharp edge of tibial tunnel exit, but also to the repetitive micromotion of the graft at the sharp edge of tunnel exit (5,28). This graft micromotion is further subdivided into two classes: the longitudinal and transverse movement, which are called “bungee effect” and “windshield–wiper effect” (29,30). Several studies have found that the two effects are associated with the length of the graft within the tibial tunnel, which the longer graft may cause more relative motion occurred between the graft and the intraarticular aperture of the tunnel (28,31). During the transtibial PCL reconstruction, long tibial tunnels can result in increased graft length within tunnel (32). In this study, the most proximal tibial tunnel approach in anterolateral tibia provides a non-differential GBA with the most distal tibial tunnel approach in anteromedial tibia. However, the TTL of the most proximal tibial tunnel approach in anterolateral tibia is approximately about 22 mm shorter than of the most distal tibial tunnel approach in anteromedial tibia. This indicate that the use of the minimum TTA in anteromedial approach requires to prepare a graft about 22 mm longer than the use of the maximum TTA in anterolateral approach. Therefore, using the most distal tibial tunnel approach in anteromedial tibia might cause more micromotion of the graft at the sharp edge of tunnel exit. The result suggests that increasing the TTA in anteromedial approach is not better for reducing the killer turn effect compared with using the anterolateral approach, even when both the method provide the same GBA. The TTL in antemedial approach is about 2.3 to 3.1 mm longer than in anterolateral approach. Because the anatomical position of the tibial PCL footprint is proximity to the popliteal neurovascular bundle, the popliteal neurovascular bundle could be easily damaged by an excessively advanced guide pin or reamer during the transtibial PCL reconstruction. In order to prevent the guide pin or reamer from intersecting with the neurovascular bundle, the drilling depth should match with the TTL while preparing the tibial tunnel. Therefore, surgeons need to know this difference and should be more careful to avoid the guide pin or reamer advancing too much to damage the neurovascular bundle in the popliteal fossa when using the anterolateral approach to perform the PCL reconstruction (33).
Limitations
Several limitations should be addressed. (I) This study only provided theoretical support for clinical practice, but the real postoperative outcomes between different tunnel approaches need to be confirmed by further clinical studies. (II) The tibial PCL attachment was located on the sagittal CT image, which might raise concerns about the precision. Actually, we could clearly identify the tibial PCL attachment after manually adjusting the grayscale value of the CT image. Besides, the digital definition of center of the PCL anterolateral and postmedial bundles’ tibial insertion by Osti et al. (34) was referred by us to ensure the accuracy of the tibial PCL attachment. (III) In this study, all the measurements were drawn from the knee extended position. The GBA might be varied as the knee flexion. As Jung et al. reported (3), there is no difference of the GBA between the knee extended position and the 90° knee flexion position. Besides, this study aimed to reveal how the GBA varied as the TTA changed and to explore the optimal tibial tunnel placement to maximize the GBA. Therefore, the position of knee joint might have little effect on relationship between the tibial tunnel position and the GBA. (IV) The data is derived from averages. The accurate GBA requires the measurement from individuals. In present study, the detailed method to measure the GBA based on the 3D knee model is provided in the method part. Researchers and doctors could refer to the method used in this study to measure the GBA for different individuals.
Conclusions
The GBA and TTL will significantly increase as the TTA becomes greater. Maximizing the TTA (50° TTA) in the anterolateral approach could provide the greatest GBA in the PCL reconstruction. No matter how the TTA is changed in the anteromedial approach, using anterolateral approach is likely to reduce the killer turn effect more effectively than using anteromedial approach.
Acknowledgments
We would like to thank John Smith (United Kingdom, 2 The Walls, St Asaph, Denbighshire, Wales) for his language assistance.
Funding: This study was supported by the National Natural Science Foundation of China (Nos. 82060413, 81874017, 81960403 and 82060405); Cuiying Scientific and Technological Innovation Program of Lanzhou University Second Hospital (No. CY2021-QN-A14); Gansu Province Science Foundation for Youths (No. 21JR1RA154); Medical Innovation and Development Project of Lanzhou University (No. lzuyxcx-2022-173) and Innovation Fund Project of Colleges and Universities in Gansu Province (No. 2022B-044).
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://qims.amegroups.com/article/view/10.21037/qims-22-1057/coif). All authors report that this work was supported by the National Natural Science Foundation of China (Nos. 82060413, 81874017, 81960403 and 82060405); Cuiying Scientific and Technological Innovation Program of Lanzhou University Second Hospital (No. CY2021-QN-A14); Gansu Province Science Foundation for Youths (No. 21JR1RA154); Medical Innovation and Development Project of Lanzhou University (No. lzuyxcx-2022-173) and Innovation Fund Project of Colleges and Universities in Gansu Province (No. 2022B-044). The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The Ethics Committee of Lanzhou University Second Hospital approved this study (No. 2021A-169), and the requirement to obtain individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Lee DY, Kim DH, Kim HJ, Ahn HS, Lee TH, Hwang SC. Posterior Cruciate Ligament Reconstruction With Transtibial or Tibial Inlay Techniques: A Meta-analysis of Biomechanical and Clinical Outcomes. Am J Sports Med 2018;46:2789-97. [Crossref] [PubMed]
- Shin YS, Kim HJ, Lee DH. No Clinically Important Difference in Knee Scores or Instability Between Transtibial and Inlay Techniques for PCL Reconstruction: A Systematic Review. Clin Orthop Relat Res 2017;475:1239-48. [Crossref] [PubMed]
- Jung M, Song SY, Cha M, Chung HM, Kim YS, Jang SW, Seo YJ. Graft bending angle of the reconstructed posterior cruciate ligament gradually decreases as knee flexion increases. Knee Surg Sports Traumatol Arthrosc 2020;28:2626-33. [Crossref] [PubMed]
- Zhang X, Teng Y, Li R, Ma C, Yang X, Wang H, Han H, Jiang J, Geng B, Wu M, Xia Y. Proximal, Distal, and Combined Fixation Within the Tibial Tunnel in Transtibial Posterior Cruciate Ligament Reconstruction: A Time-Zero Biomechanical Study In Vitro. Arthroscopy 2019;35:1667-73. [Crossref] [PubMed]
- Huang TW, Wang CJ, Weng LH, Chan YS. Reducing the "killer turn" in posterior cruciate ligament reconstruction. Arthroscopy 2003;19:712-6. [Crossref] [PubMed]
- Jia G, Tang Y, Liu Z, Peng B, Da L, Yang J, Liu X, Ma M, Han H, Wu M, Geng B, Xia Y, Teng Y. 3D Killer Turn Angle in Transtibial Posterior Cruciate Ligament Reconstruction Is Determined by the Graft Turning Angle both in the Sagittal and Coronal Planes. Orthop Surg 2022;14:2298-306. [Crossref] [PubMed]
- Kim SJ, Shin JW, Lee CH, Shin HJ, Kim SH, Jeong JH, Lee JW. Biomechanical comparisons of three different tibial tunnel directions in posterior cruciate ligament reconstruction. Arthroscopy 2005;21:286-93. [Crossref] [PubMed]
- Lee YS, Ra HJ, Ahn JH, Ha JK, Kim JG. Posterior cruciate ligament tibial insertion anatomy and implications for tibial tunnel placement. Arthroscopy 2011;27:182-7. [Crossref] [PubMed]
- Teng Y, Zhang X, Ma C, Wu H, Li R, Wang H, Han H, Xia Y. Evaluation of the permissible maximum angle of the tibial tunnel in transtibial anatomic posterior cruciate ligament reconstruction by computed tomography. Arch Orthop Trauma Surg 2019;139:547-52. [Crossref] [PubMed]
- Teng Y, Da L, Jia G, Hu J, Liu Z, Zhang S, Han H, Xia Y. What Is the Maximum Tibial Tunnel Angle for Transtibial PCL Reconstruction? A Comparison Based on Virtual Radiographs, CT Images, and 3D Knee Models. Clin Orthop Relat Res 2022;480:918-28. [Crossref] [PubMed]
- Zhang X, Teng Y, Yang X, Li R, Ma C, Wang H, Han H, Geng B, Xia Y. Evaluation of the theoretical optimal angle of the tibial tunnel in transtibial anatomic posterior cruciate ligament reconstruction by computed tomography. BMC Musculoskelet Disord 2018;19:436. [Crossref] [PubMed]
- Teng Y, Jia G, Da L, Peng B, Liu Z, Han H, Wu M, Xia Y. The Permissive Safe Angle of the Tibial Tunnel in Transtibial Posterior Cruciate Ligament Reconstruction: A Three-Dimensional Simulation Study. Orthop Surg 2022;14:1193-202. [Crossref] [PubMed]
- Shi H. The Way of Expressing, Analyzing and Calculating Space Angles in a Plane. Metal Cutting Theory. Springer; 2018:11-38.
- Ahn JH, Bae JH, Lee YS, Choi K, Bae TS, Wang JH. An anatomical and biomechanical comparison of anteromedial and anterolateral approaches for tibial tunnel of posterior cruciate ligament reconstruction: evaluation of the widening effect of the anterolateral approach. Am J Sports Med 2009;37:1777-83. [Crossref] [PubMed]
- Johannsen AM, Anderson CJ, Wijdicks CA, Engebretsen L, LaPrade RF. Radiographic landmarks for tunnel positioning in posterior cruciate ligament reconstructions. Am J Sports Med 2013;41:35-42. [Crossref] [PubMed]
- Ishikawa M, Hoo C, Ishifuro M, Kamei G, Omoto T, Kano T, Nakata K, Nekomoto A, Nakamae A, Adachi N. Application of a true lateral virtual radiograph from 3D-CT to identify the femoral reference point of the medial patellofemoral ligament. Knee Surg Sports Traumatol Arthrosc 2021;29:3809-17. [Crossref] [PubMed]
- Zhang Y, Wang J, Xiao J, Zhao L, Li ZH, Yan G, Shi ZJ. Measurement and comparison of tibial posterior slope angle in different methods based on three-dimensional reconstruction. Knee 2014;21:694-8. [Crossref] [PubMed]
- Dean RS, DePhillipo NN, Chahla J, Larson CM, LaPrade RF. Posterior Tibial Slope Measurements Using the Anatomic Axis Are Significantly Increased Compared With Those That Use the Mechanical Axis. Arthroscopy 2021;37:243-9. [Crossref] [PubMed]
- Lertwanich P, Martins CA, Asai S, Ingham SJ, Smolinski P, Fu FH. Anterior cruciate ligament tunnel position measurement reliability on 3-dimensional reconstructed computed tomography. Arthroscopy 2011;27:391-8. [Crossref] [PubMed]
- Fanelli GC, Edson CJ. Arthroscopically assisted combined anterior and posterior cruciate ligament reconstruction in the multiple ligament injured knee: 2- to 10-year follow-up. Arthroscopy 2002;18:703-14. [Crossref] [PubMed]
- Kim SJ, Chang JH, Kang YH, Song DH, Park KY. Clinical comparison of anteromedial versus anterolateral tibial tunnel direction for transtibial posterior cruciate ligament reconstruction: 2 to 8 years' follow-up. Am J Sports Med 2009;37:693-8. [Crossref] [PubMed]
- Kim SJ, Kim TE, Jo SB, Kung YP. Comparison of the clinical results of three posterior cruciate ligament reconstruction techniques. J Bone Joint Surg Am 2009;91:2543-9. [Crossref] [PubMed]
- Lin Y, Huang Z, Zhang K, Pan X, Huang X, Li J, Li Q. Lower Tibial Tunnel Placement in Isolated Posterior Cruciate Ligament Reconstruction: Clinical Outcomes and Quantitative Radiological Analysis of the Killer Turn. Orthop J Sports Med 2020;8:2325967120923950. [Crossref] [PubMed]
- May JH, Gillette BP, Morgan JA, Krych AJ, Stuart MJ, Levy BA. Transtibial versus inlay posterior cruciate ligament reconstruction: an evidence-based systematic review. J Knee Surg 2010;23:73-9. [Crossref] [PubMed]
- Ahn JH, Wang JH, Lee SH, Yoo JC, Jeon WJ. Increasing the distance between the posterior cruciate ligament and the popliteal neurovascular bundle by a limited posterior capsular release during arthroscopic transtibial posterior cruciate ligament reconstruction: a cadaveric angiographic study. Am J Sports Med 2007;35:787-92. [Crossref] [PubMed]
- Gill TJ 4th, Van de Velde SK, Carroll KM, Robertson WJ, Heyworth BE. Surgical technique: aperture fixation in PCL reconstruction: applying biomechanics to surgery. Clin Orthop Relat Res 2012;470:853-60. [Crossref] [PubMed]
- Shin YS, Han SB, Hwang YK, Suh DW, Lee DH. Tibial tunnel aperture location during single-bundle posterior cruciate ligament reconstruction: comparison of tibial guide positions. Arthroscopy 2015;31:874-81. [Crossref] [PubMed]
- Brown CH Jr, Wilson DR, Hecker AT, Ferragamo M. Graft-bone motion and tensile properties of hamstring and patellar tendon anterior cruciate ligament femoral graft fixation under cyclic loading. Arthroscopy 2004;20:922-35. [Crossref] [PubMed]
- Paessler HH, Mastrokalos DS. Anterior cruciate ligament reconstruction using semitendinosus and gracilis tendons, bone patellar tendon, or quadriceps tendon-graft with press-fit fixation without hardware. A new and innovative procedure. Orthop Clin North Am 2003;34:49-64. [Crossref] [PubMed]
- Zhu J, Marshall B, Tang X, Linde MA, Fu FH, Smolinski P. ACL graft with extra-cortical fixation rotates around the femoral tunnel aperture during knee flexion. Knee Surg Sports Traumatol Arthrosc 2022;30:116-23. [Crossref] [PubMed]
- Shen P, Li X, Xu C, Zhao S, Dong S, Zhang Y, Zhao J. Differences of Intra-Articular Graft Length between Sandwich-Style Reconstruction and Zhao-Style Non-Remnant-Preserving Double-Bundle Reconstruction of Posterior Cruciate Ligament. PLoS One 2016;11:e0155678. [Crossref] [PubMed]
- Sim JA, Kim JM, Lee S, Song EK, Seon JK. No difference in graft healing or clinical outcome between trans-portal and outside-in techniques after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 2018;26:2338-44. [Crossref] [PubMed]
- Franciozi CE, Albertoni LJ, Ribeiro FN, Moscon AC, Munhoz Mde A, Krause R, Abdalla RJ. A simple method to minimize vascular lesion of the popliteal artery by guidewire during transtibial posterior cruciate ligament reconstruction: a cadaveric study. Arthroscopy 2014;30:1124-30. [Crossref] [PubMed]
- Osti M, Hierzer D, Krawinkel A, Hoffelner T, Benedetto KP. The predictive effect of anatomic femoral and tibial graft tunnel placement in posterior cruciate ligament reconstruction on functional and radiological outcome. Int Orthop 2015;39:1181-6. [Crossref] [PubMed]


