
A series of tuberculous cold abscesses at uncommon anatomic sites
Introduction
Tuberculosis (TB) is resurging recently and still being a serious public health problem, especially in low- and middle-income countries. More than 1 million people are reported to die of TB per year (1,2).
Tuberculous cold abscesses (TCA) are less commonly seen, especially in the spleen and chest wall (3-6). Direct extension of underlying pleural, lung parenchymal, or chest wall lymphadenitis, or hematogenous dissemination resulting from activation of dormant tuberculous lesions are thought to be the main reasons of TCA (3,5,7). Timely diagnosis, prompt and appropriate treatment of TCA is crucial.
We retrospectively collected the clinicopathological and imaging findings [computed tomography (CT) and/or magnetic resonance imaging (MRI)] of a series of six TCAs, which were all misdiagnosed radiologically.
Cases description
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patients or the patients’ parents for the publication of this case report with the accompanying images. A copy of the written consent was available for review by the editorial office of this journal.
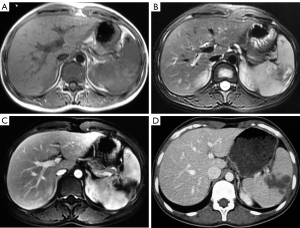
Four cases complained of a fluctuating, painless, and tenderness mass without redness of surface or swelling, and one of them with pain on the left upper limb (Table 1). One complained of intermittent fever for 20 days after trauma, and with elevated leukocyte counts. And one splenic TCA was asymptomatic and found incidentally by the ultrasound (Figure 1).
Table 1
| Case | Gender | Age | Location | Presentation | Exam | Other | Treatment |
|---|---|---|---|---|---|---|---|
| 1 | m | 14 yo | Left hip joint | Intermittent fever lasts for 20 days | CT + MRI | Erosion of the right hip and ankle joint | Aspiration and drainage, ATT |
| 2 | m | 16 yo | Right chest wall | A fluctuating, tenderness, and painless mass | MRI | Rib erosion, pulmonary tuberculosis | Excised surgically, ATT |
| 3 | f | 23 yo | Spleen | A splenic mass found on the US | CT + MRI | – | Splenectomy, ATT |
| 4 | f | 25 yo | Right iliac fossa and thigh | A massive fluctuating, tenderness, and painless mass | CT | – | Aspiration and drainage, ATT |
| 5 | f | 34 yo | Right axillary | A fluctuating, tenderness, and painless mass | MRI | – | Excised surgically, ATT |
| 6 | m | 75 yo | Left axilla | A fluctuating, tenderness, and painless mass, with pain on the left upper limb | MRI | – | Aspiration and drainage, ATT |
TCA, tuberculous cold abscesses; m, male; yo, years old; CT, computed tomography; MRI, magnetic resonance imaging; ATT, anti-tuberculosis treatment; f, female; US, ultrasound.
Their ages ranged from 14 to 75 years old, and the median age was 24 years old. Five of them were adolescents or young adults. Three males and three females were enrolled, with a gender ratio of 1:1.
The maximal size ranged from 4 to 10 cm, with an average of 6.97±2.47 cm. Their locations were the spleen (n=1), the left hip joint (n=1), the right iliac fossa and thigh (n=1), the right chest wall (n=1), and the axilla (n=2) (Table 1).
CT and MR findings
On images, they were all cystic masses, three were lobulated and three were irregular. Two presented as multi-cystic lesions, and four were mono-cystic lesions. Four were heterogeneous, and two were mainly homogeneous.
Splenic TCA showed hypo-attenuation on unenhanced CT, slightly hyper-signal intensity (SI) on T1 weighted imaging (T1WI), and heterogeneous hyper-SI on T2 weighted imaging (T2WI) with hypo-SI rim, and showed undiscernible rim enhancement of cystic wall with intra- and extra-spleen involvement (Figure 1). It was misdiagnosed as splenic neoplasm pre-splenectomy.
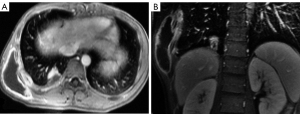
The other five cold abscesses showed hypo-attenuation on unenhanced CT, hypo-SI on T1WI, heterogeneous hyper-SI on T2WI, and notable fine rim enhancement (Figure 2). Two cases were accompanied by bone erosion (rib, hip, and ankle joint), and one with pulmonary consolidation (Figure 2). They were misdiagnosed as septic abscess, infection secondary to lymphatic malformation (LM), and soft tissue tumor, respectively.
Histological results
Three TCAs were surgically excised completely, and three cases were biopsied and drained. Microscopically, epithelioid histiocytes and multinucleated giant cells, granulation tissue, and caseous necrosis were seen. The diagnosis of TCA was made on acid-fast staining, then they all underwent anti-tuberculosis treatment (ATT).
Discussion
TCAs were mainly heterogeneous cystic masses, with fine or undiscernible rim enhancement. It mainly showed hypo-attenuation on unenhanced CT, hypo-SI on T1WI, heterogeneous hyper-SI on T2WI, and notable rim enhancement of the cystic wall.
Three males and three females were included, with a gender ratio of 1:1. It is reported that male was more commonly affected by TB, and the age-standardized incidence of the male was approximately twice as high as that of women (1). Five cases were young. Young adults are indeed more prone to TB and chest TCA (1).
Cold abscesses of the para-spinal region (psoas abscess) are more common (8), especially surrounding the lumbar and thoracic vertebrae. A painless cystic mass is the most common manifestation of splenic TCA (5). TCA can be an isolated lesion, without the involvement of other sites. The spleen, the left hip joint, the right iliac fossa and thigh, the right chest wall, and the axilla are uncommon sites. These TCAs are found in relatively large sizes. We speculate that it may be due to most TCAs being asymptomatic (without fever or pain or pulmonary involvement).
Pyogenic abscess, splenic neoplasm, LM, or chest wall tumor (especially bone and soft tissue tumor), should be taken into consideration in the differentiation of TCAs (9). TCA commonly shows fine or undiscernible cystic walls, which was unlike the pyogenic abscess or secondary infection of LM. Bacterial abscesses were common with thickened abscess walls, with the elevation of white cell count.
For these cases included in this review, three TCAs were surgically excised completely, and three cases were biopsied and drained, then they all underwent ATT. The combination of anti-tubercular medication and surgical excision was thought to be an effective treatment for chest TB cold abscesses (3,4), and CT-guided percutaneous aspiration and drainage may serve as another treatment option (8). Deng et al. even proposed the ‘6C+A’ strategy, which was believed to reduce the rate of recurrence and complications of chest TCA (7).
Positive acid-fast staining, positive Lowenstein-Jensen culture, granulomatous with caseous necrosis on the histological result, or positive polymerase chain reaction (PCR) for Mycobacterium tuberculosis were the methods to confirm the diagnosis of TB (3,7,10).
Conclusions
TCA often presents as lobulated or irregular cystic masses, seldom with fever and elevation of leukocyte counts, may be accompanied by erosion of surrounding bone and pulmonary TB, and was easily misdiagnosed. It mainly showed hypo-attenuation on unenhanced CT, hypo-SI on T1WI, heterogeneous hyper-SI on T2WI, and notable fine rim enhancement. Combined the clinical and imaging (CT and/or MR) findings frequently invoke the diagnosis of TCA.
Acknowledgments
Funding: This research was supported by grants from the Science and Technology Council of Shanghai (No. 18140901200), and the Medical Specialty Construction of Minhang District (No. 2020MWFC05).
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://qims.amegroups.com/article/view/10.21037/qims-22-743/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patients or the patients’ parents for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- The global burden of tuberculosis: results from the Global Burden of Disease Study 2015. Lancet Infect Dis 2018;18:261-84. [Crossref] [PubMed]
- Murray CJ, Ortblad KF, Guinovart C, Lim SS, Wolock TM, Roberts DA, et al. Global, regional, and national incidence and mortality for HIV, tuberculosis, and malaria during 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2014;384:1005-70. [Crossref] [PubMed]
- Cho KD, Cho DG, Jo MS, Ahn MI, Park CB. Current surgical therapy for patients with tuberculous abscess of the chest wall. Ann Thorac Surg 2006;81:1220-6. [Crossref] [PubMed]
- Dv K, Gunasekaran K, Mishra AK, Iyyadurai R. Disseminated tuberculosis presenting as cold abscess of the thyroid gland-a case report. Oxf Med Case Reports 2017;2017:omx049. [Crossref] [PubMed]
- Kabiri EH, Alassane EA, Kamdem MK, Bhairis M, Amraoui M, El Oueriachi F, El Hammoumi M. Tuberculous cold abscess of the chest wall: A clinical and surgical experience. Report of 16 cases(Case series). Ann Med Surg (Lond) 2020;51:54-8. [Crossref] [PubMed]
- Grover S, Arya Y, Gaba S, Gupta M, Syal A. Isolated Splenic Tuberculosis: A Diagnostic Conundrum. Cureus 2021;13:e12958. [PubMed]
- Deng B, Tan QY, Wang RW, He Y, Jiang YG, Zhou JH, Liang YG. Surgical strategy for tubercular abscess in the chest wall: experience of 120 cases. Eur J Cardiothorac Surg 2012;41:1349-52. [Crossref] [PubMed]
- Tsagouli P, Sotiropoulou E, Filippousis P, Sidiropoulou N, Georgiadi V, Thanos L. Contribution of computed tomography guided percutaneous drainage of tuberculous cold abscesses adjunctive to pharmaceutical anti-tubercular treatment. Eur J Radiol 2012;81:562-5. [Crossref] [PubMed]
- Sonhaye L, Amadou A, Gnandi-Piou F, Assih K, Tchaou M, Kolou B, Adambounou K, N'Timon B, Agoda-Koussema L, Adjenou K, N'Dakena K. Tuberculous Abscess of the Chest Wall Simulate Pyogenic Abscess. Case Rep Radiol 2015;2015:195412. [Crossref] [PubMed]
- Hsu HE, Chen CY. Tuberculous retropharyngeal abscess with Pott disease and tuberculous abscess of the chest wall: A case report. Medicine (Baltimore) 2019;98:e16280. [Crossref] [PubMed]


