
Distance between the C2 vertical line and the femoral heads: a quasi-invariant global sagittal alignment parameter in both standing and sitting positions for asymptomatic adults
Introduction
Dubousset’s widely accepted concept that “the entire pelvis is a vertebra” triggered a considerable number of investigations into the relationship between spinal sagittal alignment and pelvic morphology (1). The spine sagittal study began as research examining the correlation between pelvic and spine radiographic parameters but has grown into a study of global sagittal balance, which involves assessing the connection between the cervical spine and the remainder of the skeleton, even as far down as the ankles (2-6). Global sagittal malalignment is closely related to the occurrence of low back pain and the emergence of proximal junctional kyphosis (PJK) after spinal surgery (7,8). Proper restoration of global sagittal alignment is essential for reducing mechanical complications after surgery for adult spinal deformities.
Global sagittal alignment is most generally quantified by measuring the sagittal vertical axis (SVA). However, one important caveat that should be taken into account is that SVA is affected by pelvic rotation and patient position (1). Kim and colleagues proposed a radiologic parameter similar to SVA, cranial sagittal vertical axis (CrSVA), to evaluate global sagittal alignment. CrSVA is defined as the displacement from the cranial center of mass to the sacrum (CrSVA-S), to the hip center (CrSVA-H), to the knee center (CrSVA-K), or to the ankle center (CrSVA-A) (9). Other angular parameters, including the T1-pelvic angle (TPA) and global sagittal angle (GSA), were additionally proposed by Schwab and colleagues (10,11). However, the abovementioned parameters are variable in the population, and the ideal range of these parameters is too large to be established as the target of correction. Therefore, a novel radiographic parameter is still needed to serve as the correction target for adult spinal deformities.
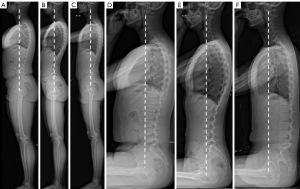
Recently, a new parameter, the distance between the C2 vertical line and the femoral heads (C2-FH), was proposed by Shu et al. (12). Specifically, it is defined as the distance between the vertical line of the center of the C2 vertebra and the centers of the 2 femoral heads (Figure 1). Different from the traditional parameters, the stability of C2-FH in the population is its most notable feature. The study by Shu et al. showed that C2-FH is approximately 1 cm on average in the standing position, and it is not related to age (12). C2-FH is similar to a previously reported 3D parameter, cervical spine with odontoid hip axis angle (OD-HA) (13,14), which is measured on EOS 3D images. OD-HA has been reported to be a “quasi-invariant” parameter in both young asymptomatic adults (13) and asymptomatic adults older than 49 years (15). Similar to OD-HA (13), C2-FH was also reported to be a less variable (quasi-invariant) parameter, which is in accordance with the concept of the “cone of economy (CoE)” proposed by Prof. Dubousset. The CoE describes a physical state in which the body can maintain balance without external support, obtain the best upright posture, and minimize energy consumption in a narrow range (16). Thus, the body tends to stay in the most energy-saving posture to minimize energy consumption. Apart from the standing position, the CoE concept should also be applicable to the free-sitting position. Previous studies have shown that the sitting position involves a unique sagittal alignment and compensation mechanism, and the study of asymptomatic adults in sitting position is conducive to the sagittal reconstruction of patients undergoing spinal surgery (17,18). The purpose of this study was to verify whether C2-FH is also quasi-invariant in the sitting position and to investigate the transitional change in global spinal alignment from the standing to sitting position. We present this article in accordance with the STROBE reporting checklist (available at https://qims.amegroups.com/article/view/10.21037/qims-22-1160/rc).

Methods
Participants
A cross-sectional, prospective study design was employed. Between February 1, 2020, and February 31, 2020, 59 asymptomatic volunteers were prospectively recruited (Figure 2). The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013) and was approved by the Ethics Committee of The Affiliated Drum Tower Hospital of Nanjing University Medical School (No. 2021-LCYJ-DBZ-05). Informed consent was obtained from all volunteers regarding the study protocol's risks, purposes, and methods. The inclusion criteria were as follows: age between 18 and 35 years and no symptoms related to neck or back pain. The exclusion criteria were as follows: a history of any prior lower extremity or spine surgery; and a history of inflammatory arthritis, neuromuscular disorders, or congenital anomalies. Individuals were divided into the following 3 groups according to the percentile of Δ pelvic tilt (PT) (PT difference between standing position and sitting position): group A (1–25% ΔPT, n=14), group B (25–75% ΔPT, n=30), and group C (75–100% ΔPT, n=15). This means that the pelvic retroversion change increased from group A to group C. The subgroup analysis was aimed at clarifying whether the difference in pelvic retroversion from the standing to sitting position would change the quasi-invariant C2-FH in the sitting position.
Data collection
All participants underwent full-body lateral standing and sitting radiography imaging (EOS Imaging, Paris, France; voltage: 110–240 V; frequency: 50 Hz/60 Hz; absorbed power: 303 W). The protocol included a comfortable weight-bearing, free-standing, and sitting posture with arms flexed at 45 degrees to avoid superimposition with the spine (19).
A senior spinal surgeon and a radiologist with experience diagnosing skeletal diseases with Surgimap (Nemaris Inc., New York, NY, USA) measured all radiological parameters. The following radiographical parameters were evaluated: T4–T12 thoracic kyphosis (TK), defined as the angle between the upper endplate of the T4 and the lower endplate of the T12; cervical lordosis (CL), defined as the angle between the upper endplate of the C2 and the lower endplate of C7; lumbar lordosis (LL), defined as the angle between the upper endplate of the L1 and the upper endplate of the S1; L1–L4 lordosis, defined as the angle between the upper endplate of the L1 and the lower endplate of L4; L4–S1 lordosis, defined as the angle between the upper endplate of the L4 and the upper endplate of the S1; pelvic incidence (PI); pelvic tilt (PT); sacral slope (SS); SVA, defined as the offset between the vertical plumb line from the posterior edge of the base of the sacrum and the center of the C7 vertebra; T1–pelvic angle (TPA), defined as the angle subtended by lines drawn from the center of the femoral head axis to the center of the T1 vertebral body and to the middle of the S1 endplate; C2-FH, defined as the distance between the C2 vertical line to the femoral heads; and the angle of each lumbar disc.
There were no missing data in this study.
Statistical analysis
Statistical analysis and processing of data were completed using SPSS 23.0 (IBM Corp., Armonk, NY, USA). Average values are reported as the mean (M) and SD. For C2-FH, a parameter was classified as normal if within M ± 1 × SD range, subnormal high if between M + 1 × SD and M + 2 × SD (and low if between M − 1 × SD and M − 2 × SD), or abnormal if out of the range of M ± 2 × SD (high or low) (15). Summary statistics calculated using analysis of variance (ANOVA) were used to provide 95% confidence intervals for measurement errors. Comparison of the dependent variables among the 3 groups was also conducted using ANOVA. Statistical significance was set at P<0.05 in all analyses.
Results
The average age of the 59 participants (43 men and 16 women) was 25.6±2.1 years (range, 21–32 years). The mean age of the men was 25.6±1.8 years (range, 23–30 years), which was comparable to that of the women (25.7±2.9 years; P=0.867). All radiographic parameters, except PI, were significantly different from the standing to sitting position (Table 1).
Table 1
| Variable | Standing | Sitting | Δ Standing and sitting | 95% CI | P value |
|---|---|---|---|---|---|
| Age (years) | 25.6±2.1 | 25.6±2.1 | – | – | – |
| Participant, n | 59 | 59 | – | – | – |
| Female | 16 | 16 | – | – | – |
| Male | 43 | 43 | – | – | – |
| BMI (kg/m2) | 25.5±2.7 | 25.5±2.7 | – | – | – |
| C2-FH (mm) | −11.95±21.33 | −1.01±21.62 | −10.17±22.86 | −20.486 to −3.893 | 0.008 |
| TK (°) | 25.58±9.20 | 20.67±10.81 | 4.82±6.39 | 18.098 to 25.170 | 0.01 |
| CL (°) | 5.02±12.5 | −0.48±9.73 | 5.5±2.87 | 2.628 to 7.325 | <0.001 |
| LL (°) | −46.94±10.26 | −21.67±15.89 | −26.20±16.88 | −41.737 to −26.479 | <0.001 |
| PT (°) | 8.52±6.04 | 24.94±11.49 | −16.42±10.11 | 11.352 to 18.648 | <0.001 |
| PI (°) | 44.09±9.04 | 44.95±9.43 | −0.86±2.85 | 37.831 to 49.319 | 0.61 |
| SS (°) | 35.57±7.24 | 20.02±10.64 | 15.55±10.17 | 25.199 to 31.951 | <0.001 |
| SVA (mm) | −1.03±23.47 | 41.01±29.08 | −41.37±31.21 | 6.454 to 37.879 | <0.001 |
| TPA (°) | 4.79±6.07 | 22.19±12.09 | −17.39±10.97 | 5.858 to 16.976 | <0.001 |
| L1-L4 (°) | 15.28±9.13 | −6.69±12.55 | −8.59±10.74 | −9.087 to 2.887 | <0.001 |
| L4-S1 (°) | −34.66±6.72 | −16.11±8.11 | −18.55±8.86 | −25.532 to −17.751 | <0.001 |
| ΔPT/PI | 0.18±0.12 | 0.55±0.23 | −0.37±0.22 | 0.133 to 0.254 | <0.001 |
| ΔPI-LL | −2.84±9.44 | 22.20±15.01 | −25.05±14.14 | 1.625 to 17.308 | <0.001 |
Data are presented as mean ± standard deviation. BMI, body mass index; C2-FH, the distance from the C2 vertical line to the femoral heads; CL, cervical lordosis; TK, thoracic kyphosis; LL, lumbar lordosis; PT, pelvic tilt; PI, pelvic incidence; SS, sacral slope; SVA, sagittal vertical axis; TPA, T1-pelvic angle.
The radiographic parameters were compared among the 3 subgroups based on the percentile of ΔPT (ΔPT group A: −5.99; ΔPT group B: −14.32; ΔPT group C: −30.35) in both the standing (Table 2) and sitting positions (Table 3) to investigate whether the degree of pelvic rotation change would impact the radiographic parameters. As shown in Table 2, there was no significant difference in any parameter among the 3 groups in the standing position. As shown in Table 2, there was no significant difference in any parameter among the 3 groups in the standing position. In the sitting position, for different degrees of pelvic retroversion, the 3 groups showed significant differences in the other parameters except for C2-FH (P=0.80; 95% CI: −20.486 to −3.893), CL (P=0.47; 95% CI: −5.645 to 4.964), TK (P=0.54; 95% CI: 17.058–25.1), and PI (P=0.44; 95% CI: 40.747–49.087). Surprisingly, C2-FH differed slightly between the 3 groups in both the standing (P=0.87) and sitting (P=0.80) positions. For C2-FH, with 67% of participants within the normal range, we considered C2-FH to be “quasi-invariant”.
Table 2
| Standing | Group A | Group B | Group C | 95% CI | P value |
|---|---|---|---|---|---|
| Participant, n | 14 | 30 | 15 | – | – |
| C2-FH (mm) | −8.69±19.27 | −12.19±21.81 | −14.69±23.38 | −22.546 to 1.163 | 0.87 |
| TK (°) | 25.67±9.12 | 26.32±10.35 | 24.06±7.01 | 21.320 to 32.263 | 0.74 |
| CL (°) | 4.88±11.5 | 5.17±10.72 | 4.77±13.46 | 1.706 to 7.867 | 0.78 |
| LL (°) | −45.39±9.22 | −45.58±9.48 | −51.09±12.09 | −51.339 to −38.694 | 0.19 |
| PT (°) | 8.08±5.62 | 8.94±6.62 | 8.09±5.50 | 5.325 to 12.475 | 0.86 |
| PI (°) | 42.66±8.50 | 43.46±9.97 | 46.69±7.43 | 37.428 to 48.955 | 0.42 |
| SS (°) | 34.57±5.45 | 34.52±7.99 | 38.61±6.65 | 30.704 to 37.846 | 0.17 |
| SVA (mm) | 4.73±20.68 | −0.79±20.91 | −7.78±31.05 | −8.640 to 18.757 | 0.38 |
| TPA (°) | 4.84±5.87 | 5.10±6.29 | 4.15±6.19 | 1.471 to 9.329 | 0.88 |
| L1-L4 (°) | −15.32±7.83 | −14.44±9.49 | −16.93±9.86 | −20.408 to −9.642 | 0.69 |
| L4-S1 (°) | −32.35±7.25 | −34.50±4.95 | −37.13±8.70 | −36.726 to −26.891 | 0.15 |
| ΔPT/PI | 0.18±0.10 | 0.20±0.13 | 0.17±0.11 | 0.133 to 0.254 | 0.77 |
| ΔPI-LL | −2.72±10.05 | −2.12±9.86 | −4.40±8.38 | −8.505 to 4.855 | 0.75 |
Data are presented as mean ± standard deviation. Group A: 1–25% ΔPT; group B: 25–75% ΔPT; group C: 75–100% ΔPT. C2-FH, the distance from the C2 vertical line to the femoral heads; CL, cervical lordosis; TK, thoracic kyphosis; LL, lumbar lordosis; PT, pelvic tilt; PI, pelvic incidence; SS, sacral slope; SVA, sagittal vertical axis; TPA, T1-pelvic angle.
Table 3
| Sitting | Group A | Group B | Group C | 95% CI | P value |
|---|---|---|---|---|---|
| Participant, n | 14 | 30 | 15 | – | – |
| C2-FH (mm) | −0.38±18.71 | −1.45±23.98 | −0.69±20.45 | −20.486 to −3.893 | 0.80 |
| TK (°) | 22.49±11.66 | 21.08±10.57 | 18.19±10.74 | 17.058 to 25.100 | 0.54 |
| CL (°) | 2.14±11.62 | −0.18±8.73 | −1.2±10.98 | −5.645 to 4.964 | 0.47 |
| LL (°) | −34.89±11.89 | −23.73±12.71 | −5.23±10.31 | −28.819 to −19.009 | <0.001 |
| PT (°) | 14.06±6.00 | 23.26±7.81 | 38.43±8.24 | 20.247 to 26.291 | <0.001 |
| PI (°) | 42.79±8.71 | 44.80±10.79 | 47.29±6.77 | 40.747 to 49.087 | 0.44 |
| SS (°) | 28.72±4.90 | 21.55±9.39 | 8.85±7.07 | 18.030 to 25.287 | <0.001 |
| SVA (mm) | 20.26±24.65 | 40.64±22.63 | 59.73±32.99 | 31.900 to 49.417 | <0.001 |
| TPA (°) | 10.64±8.33 | 20.82±7.31 | 35.71±9.85 | 18.019 to 23.678 | <0.001 |
| L1-L4 (°) | −13.81±9.24 | −9.30±11.29 | 5.17±9.64 | −13.809 to −5.088 | <0.001 |
| L4-S1 (°) | −23.06±6.84 | −15.84±6.80 | −10.16±6.84 | −18.533 to −13.274 | <0.001 |
| ΔPT/PI | 0.32±0.09 | 0.53±0.15 | 0.82±0.15 | 0.467 to 0.586 | <0.001 |
| ΔPI-LL | 7.90±12.25 | 21.15±10.97 | 37.67±9.06 | 16.838 to 25.327 | <0.001 |
Data are presented as mean ± standard deviation. Group A: 1–25% ΔPT; group B: 25–75% ΔPT; group C: 75–100% ΔPT. C2-FH, the distance from the C2 vertical line to the femoral heads; CL, cervical lordosis; TK, thoracic kyphosis; LL, lumbar lordosis; PT, pelvic tilt; PI, pelvic incidence; SS, sacral slope; SVA, sagittal vertical axis; TPA, T1-pelvic angle.
The changes in radiographic parameters from standing to sitting positions among the 3 subgroups are shown in Table 4. As ΔPT gradually increased, ΔSS, ΔLL, ΔSVA, ΔL1-L4, ΔL4-S1, ΔTPA, ΔPT/PI, and ΔPI-LL showed corresponding gradual changes (all P values <0.05). However, there was no significant difference in PI (P=0.39), CL (P=0.46), C2-FH (P=0.51), or TK (P=0.51).
Table 4
| Δ Standing and sitting | Group A | Group B | Group C | 95% CI | P value |
|---|---|---|---|---|---|
| Participant, n | 14 | 30 | 15 | – | – |
| ΔC2-FH (mm) | −7.71±22.48 | −10.38±23.16 | −12.03±23.99 | −28.811 to −0.558 | 0.75 |
| ΔTK (°) | 3.18±4.63 | 5.07±6.61 | 5.87±7.42 | 0.659 to 10.218 | 0.51 |
| ΔCL (°) | 2.74±2.96 | 5.35±2.08 | 5.97±2.48 | 6.253 to 3.045 | 0.46 |
| ΔLL (°) | −14.44±19.20 | −21.85±7.07 | −45.87±11.90 | −24.223 to −18.894 | <0.001 |
| ΔPT (°) | −5.99±2.29 | −14.32±3.69 | −30.35±8.04 | −34.007 to −24.347 | <0.001 |
| ΔPI (°) | −0.12±3.22 | −1.34±2.80 | −0.60±2.60 | −1.845 to 1.322 | 0.39 |
| ΔSS (°) | 5.85±4.04 | 12.98±4.47 | 29.76±6.84 | 24.700 to 33.146 | <0.001 |
| ΔSVA (mm) | −16.52±25.90 | −41.43±23.40 | −64.30±34.25 | −61.108 to −40.921 | <0.001 |
| ΔTPA (°) | −5.80±4.85 | −15.72±3.89 | −31.56±9.51 | −17.204 to −14.196 | <0.001 |
| ΔL1-L4 (°) | −3.14±8.93 | −5.14±5.80 | −22.11±10.78 | −14.067 to −6.938 | <0.001 |
| ΔL4-S1 (°) | −11.94±12.87 | −18.65±6.55 | −26.97±6.34 | −21.189 to −16.115 | <0.001 |
| ΔPT/PI | −0.14±0.06 | −0.33±0.12 | −0.65±0.17 | −0.378 to −0.284 | <0.001 |
| ΔPI-LL | −10.62±6.52 | −23.27±7.17 | −42.07±12.52 | −25.695 to −20.278 | <0.001 |
Data are presented as mean ± standard deviation. Group A: 1–25% ΔPT; group B: 25–75% ΔPT; group C: 75–100% ΔPT. C2-FH, the distance from the C2 vertical line to the femoral heads; CL, cervical lordosis; TK, thoracic kyphosis; LL, lumbar lordosis; PT, pelvic tilt; PI, pelvic incidence; SS, sacral slope; SVA, sagittal vertical axis; TPA, T1-pelvic angle.
Discussion
Our understanding of global sagittal morphology and its correlation with clinical outcomes and quality of life continues to evolve. As extraordinarily sophisticated EOS photography systems continue to be improved and in-depth research on global sagittal morphology continues to be conducted, attention to and comprehension of the sagittal alignment of the sitting position have increased in recent years. A more comprehensive study of global sagittal alignment in the standing and sitting positions will be advantageous for the reconstruction of global sagittal morphology and reduce mechanical complications after surgery for adult spinal deformities.
Our results showed that C2-FH is quasi-invariant in the standing position and in the sitting position across asymptomatic individuals (Figure 3). Traditional global sagittal parameters, such as SVA, CrSVA, TPA and GSA, change not only with age but also with position (20-22). The C2-SVA is a recently proposed global sagittal parameter, but it is not quasi-invariant because the posterior edge of the sacrum changes with position. In addition, the C2-SVA also changes with age and between sexes (23). OD-HA is a parameter that is very similar to C2-FH. However, previous studies have not examined the stability of OD-HA in the sitting position. Furthermore, OD-HA is a 3D angular parameter, the measurement of which requires EOS 3D reconstruction images; thus, OD-HA cannot be measured on regular standing position spine X-rays. On the other hand, C2-FH can be easily measured on regular X-rays without the requirement of EOS imaging systems. As it only considers the thoracolumbar spinal column, the C7-SVA is not sufficient for assessing global spinal balance, as it does not consider the cervical spine. To overcome the shortcomings of the C7-SVA, Kim et al. (9) proposed the CrSVA, which includes cervical alignment. However, the CrSVA has only been reported in patients with adult spinal deformity (ASD), while the normative value has not been fully reported. In addition, the cranial center of mass (CCOM) is difficult to identify on X-rays. The C2-FH proposed in this study showed excellent consistency in the asymptomatic population and in both the standing and sitting positions. The measurement of C2-FH requires only the C2 vertebra and the femoral heads, which can be clearly visualized on X-rays, and thus, the measurement could be an option when long cassette films cannot incorporate the femoral heads and the skull simultaneously, especially in the intraoperative setting.
Interestingly, the C2 vertebra tended to be above the center of the femoral heads in both the standing and sitting positions. As described by the CoE theory, the human body does little work and consumes little energy when it is upright in a narrow position. Vaz et al. confirmed that the gravity line falls over the femoral heads in many healthy volunteers (24). In 2006, Schwab et al. further demonstrated that the gravity line offset from the heels remains fixed, independent of individual age (25). In their opinion, the acetabulum is the most reliable radiographic marker of the gravity line. In line with this, we believe C2-FH may be a radiographic reflection of the equilibrium state. This hypothesis and inference are also closely related to the natural history of human evolution. The biomechanics of the human spine and pelvis are unique in nature; that is, humans have a distinctive combination of fully upright bipedal ambulation and completely vertical sagittal spinopelvic alignment (26). As early as 1950, anthropologist Sherwood Washburn asserted that the morphologic changes of the pelvis were a critical step in the evolution of humans toward permanent bipedalism (27). According to several studies of the sagittal spinopelvic morphology of the human spine, the pelvis plays a critical role in regulating the sagittal alignment of each part of the spine to keep the head and body's center of gravity straight above the femoral heads (28,29).
Our study also revealed that C2-FH in the standing position and sitting position and the change between standing and sitting were similar across the 3 subgroups based on ΔPT, indicating that the consistency in C2-FH is not perturbed by pelvic rotation (including anteversion and retroversion). This means that the sagittal spinal curves can adjust to the pelvic shape and maintain global sagittal alignment in a variety of pelvic retroversion degrees. It appears that group A might have exhibited limited pelvic retroversion during the change from standing to sitting due to the smaller average ΔPT value. It is also possible that spinal stiffness was involved. Whole-body balance relies on creating adequate lordosis to balance kyphosis, and vice versa. The change in lordosis at both the lumbar region and thoracolumbar region due to pelvic retroversion requires adaptative changes in thoracic kyphosis and the corresponding change in cervical lordosis (30). Proponents of global sagittal balance believe that changes in any of the radiographic parameters that compose the sagittal alignment induce changes in the adjacent structures because these structures compensate for these changes. These changes occur not only in the movable spinal segments but also in the pelvis and lower limbs. Therefore, the consistency of C2-FH could be maintained by the complex interaction of various parts of the sagittal plane.
Previous studies have reported that shifts from standing to sitting cause changes in the pelvis and lumbar region on radiographs, which may be interpreted as pelvic retroversion (increased PT) and a straighter lumbar curvature (decreased LL) (31,32). In the normal sitting posture, the PT correlates most closely with other spinal regions, except for the trunk and neck angles (33). This study analyzed the changes in other sagittal parameters with different PT changes from standing to sitting positions. The regional sagittal parameters, SS and LL, and the global sagittal parameter, TPA, were significantly smaller in the participants with less PT change from the standing to sitting positions. Because of the quantitative relationship between PI, SS, and PT (PI = PT + SS), the change in SS decreases as ΔPT decreases. Compared with PT, LL is more closely related to SS, so a decrease in SS will lead to a decrease in LL. TPA, as an angular parameter, is measured by 2 lines: from the center of the femoral head axis to the middle of the S1 endplate and to the center of the T1 vertebral body. The line from the center of the femoral head axis to the center of the T1 vertebral body is similar to a fixed vertical line. Because the trunk remained “vertical” in this specific study and because TPA is the sum of PT and the T1 spinopelvic inclination angle (T1SPi), it follows that TPA decreases as ΔPT decreases.
A quasi-invariant C2-FH may serve as a reference value for the surgical decision-making process for patients with ASD since optimal sagittal restoration for these patients is essential in relieving clinical outcomes (12,34,35). Among the longstanding complications of spine corrective operations is PJK, whose incidence has been reported to be as high as 62%, with several studies having evaluated its classification, risk factors, and pathogenic mechanisms (11,36-38). The relationship between changes in radiographic parameters (such as overcorrection or under correction of LL, postoperatively larger SVA) and PJK has been reported, but further clarification is still needed. The C2-FH parameter may provide insight into the occurrence of PJK since C2-FH in this study tended to be quasi-invariant in both the standing and sitting positions. In other words, the body needs to rebalance if the postoperative C2-FH is not within the normal range, and the compensation may only be present at the unfused level, which may lead to PJK during follow-up. In a recent systematic review (39), Cerpa and colleagues proposed that in an ideal postoperative global sagittal alignment, a vertical line from the CrSVA should bisect the hip joints. This is very similar to our hypothesis positing that an ideal C2-FH (C2 over the femoral heads) should be achieved after surgery for patients with ASD.
Despite the detailed information described above, this study has some limitations. First, the small sample size included in this study may reduce its power. Second, the relationship between C2-FH and health-related quality of life was not further evaluated in patients with ASD. Third, whether C2-FH changes with aging of the spine was not investigated. Finally, the intraoperative application value of C2-FH is limited.
Conclusions
C2-FH is a quasi-invariant parameter in both the standing and sitting positions for asymptomatic adults. The mean value of C2-FH was found to be −11.95 mm in the standing position and –1.01 mm in the sitting position. Stable C2-FH may serve as a reference during the surgical decision-making process in adults with spinal deformity and sagittal malalignment.
Acknowledgments
Funding: This work was financially supported by Jiangsu Provincial Key Medical Center (No. YXZXA2016009).
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://qims.amegroups.com/article/view/10.21037/qims-22-1160/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://qims.amegroups.com/article/view/10.21037/qims-22-1160/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committee of The Affiliated Drum Tower Hospital of Nanjing University Medical School (No. 2021-LCYJ-DBZ-05). Informed consent was obtained from all volunteers regarding the study protocol's risks, purposes, and methods.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Zeller RD, Ghanem I, Miladi L, Dubousset J. Posterior spinal fusion in neuromuscular scoliosis using a tibial strut graft. Results of a long-term follow-up. Spine (Phila Pa 1976) 1994;19:1628-31. [Crossref] [PubMed]
- Ilharreborde B. Sagittal balance and idiopathic scoliosis: does final sagittal alignment influence outcomes, degeneration rate or failure rate? Eur Spine J 2018;27:48-58. [Crossref] [PubMed]
- Schwab JH. Global sagittal alignment. Skeletal Radiol 2017;46:1613-4. [Crossref] [PubMed]
- Le Huec JC, Thompson W, Mohsinaly Y, Barrey C, Faundez A. Sagittal balance of the spine. Eur Spine J 2019;28:1889-905. [Crossref] [PubMed]
- Takayama K, Nakamura H, Matsuda H. Low back pain in patients treated surgically for scoliosis: longer than sixteen-year follow-up. Spine (Phila Pa 1976) 2009;34:2198-204. [Crossref] [PubMed]
- Bernstein P, Hentschel S, Platzek I, Hühne S, Ettrich U, Hartmann A, Seifert J. Thoracal flat back is a risk factor for lumbar disc degeneration after scoliosis surgery. Spine J 2014;14:925-32. [Crossref] [PubMed]
- Reames DL, Kasliwal MK, Smith JS, Hamilton DK, Arlet V, Shaffrey CI. Time to development, clinical and radiographic characteristics, and management of proximal junctional kyphosis following adult thoracolumbar instrumented fusion for spinal deformity. J Spinal Disord Tech 2015;28:E106-14. [Crossref] [PubMed]
- Alshabab BS, Lafage R, Smith JS, Kim HJ, Mundis G, Klineberg E, Shaffrey C, Daniels A, Ames C, Gupta M, Burton D, Hostin R, Bess S, Schwab F, Lafage V. Evolution of Proximal Junctional Kyphosis and Proximal Junctional Failure Rates Over 10 Years of Enrollment in a Prospective Multicenter Adult Spinal Deformity Database. Spine (Phila Pa 1976) 2022;47:922-30. [Crossref] [PubMed]
- Kim YC, Lenke LG, Lee SJ, Gum JL, Wilartratsami S, Blanke KM. The cranial sagittal vertical axis (CrSVA) is a better radiographic measure to predict clinical outcomes in adult spinal deformity surgery than the C7 SVA: a monocentric study. Eur Spine J 2017;26:2167-75. [Crossref] [PubMed]
- Protopsaltis T, Schwab F, Bronsard N, Smith JS, Klineberg E, Mundis G, Ryan DJ, Hostin R, Hart R, Burton D, Ames C, Shaffrey C, Bess S, Errico T, Lafage V. TheT1 pelvic angle, a novel radiographic measure of global sagittal deformity, accounts for both spinal inclination and pelvic tilt and correlates with health-related quality of life. J Bone Joint Surg Am 2014;96:1631-40. [Crossref] [PubMed]
- Diebo BG, Oren JH, Challier V, Lafage R, Ferrero E, Liu S, Vira S, Spiegel MA, Harris BY, Liabaud B, Henry JK, Errico TJ, Schwab FJ, Lafage V. Global sagittal axis: a step toward full-body assessment of sagittal plane deformity in the human body. J Neurosurg Spine 2016;25:494-9. [Crossref] [PubMed]
- Shu S, Hu Z, Bao H, Shi J, Hu A, Grelat M, Liu Z, Sun X, Qian B, Cheng JCY, Lam TP, Chu WWC, Qiu Y, Zhu Z. An analysis of the interactions between the spine, pelvis, and lower limbs in asymptomatic adults with limited pelvic compensation. Quant Imaging Med Surg 2020;10:999-1007. [Crossref] [PubMed]
- Amabile C, Pillet H, Lafage V, Barrey C, Vital JM, Skalli W. A new quasi-invariant parameter characterizing the postural alignment of young asymptomatic adults. Eur Spine J 2016;25:3666-74. [Crossref] [PubMed]
- Hu Z, Vergari C, Gajny L, Man GC, Yeung KH, Liu Z, Lam TP, Zhu Z, Qiu Y, Chu WC, Cheng JC, Skalli W. An analysis on the determinants of head to pelvic balance in a Chinese adult population. Quant Imaging Med Surg 2022;12:2311-20. [Crossref] [PubMed]
- Amabile C, Le Huec JC, Skalli W. Invariance of head-pelvis alignment and compensatory mechanisms for asymptomatic adults older than 49 years. Eur Spine J 2018;27:458-66. [Crossref] [PubMed]
- Jackson RP, Hales C. Congruent spinopelvic alignment on standing lateral radiographs of adult volunteers. Spine (Phila Pa 1976) 2000;25:2808-15. [Crossref] [PubMed]
- Nishida N, Izumiyama T, Asahi R, Iwanaga H, Yamagata H, Mihara A, Nakashima D, Imajo Y, Suzuki H, Funaba M, Sugimoto S, Fukushima M, Sakai T. Changes in the global spine alignment in the sitting position in an automobile. Spine J 2020;20:614-20. [Crossref] [PubMed]
- Sun Z, Zhou S, Jiang S, Zou D, Yu M, Li W. Variations of Sagittal Alignment in Standing Versus Sitting Positions Under the Roussouly Classification in Asymptomatic Subjects. Global Spine J 2022;12:772-9. [Crossref] [PubMed]
- Lee SH, Son ES, Seo EM, Suk KS, Kim KT. Factors determining cervical spine sagittal balance in asymptomatic adults: correlation with spinopelvic balance and thoracic inlet alignment. Spine J 2015;15:705-12. [Crossref] [PubMed]
- Chen X, Xu L, Qiu Y, Chen ZH, Zhu ZZ, Li S, Sun X. Incidence, Risk Factors, and Evolution of Proximal Junctional Kyphosis After Posterior Hemivertebra Resection and Short Fusion in Young Children With Congenital Scoliosis. Spine (Phila Pa 1976) 2018;43:1193-200. [Crossref] [PubMed]
- Pennington Z, Cottrill E, Ahmed AK, Passias P, Protopsaltis T, Neuman B, Kebaish KM, Ehresman J, Westbroek EM, Goodwin ML, Sciubba DM. Paraspinal muscle size as an independent risk factor for proximal junctional kyphosis in patients undergoing thoracolumbar fusion. J Neurosurg Spine 2019;31:380-8. [Crossref] [PubMed]
- Wang T, Zhao Y, Liang Y, Zhang H, Wang Z, Wang Y. Risk factor analysis of proximal junctional kyphosis after posterior osteotomy in patients with ankylosing spondylitis. J Neurosurg Spine 2018;29:75-80. [Crossref] [PubMed]
- Charles YP, Bauduin E, Pesenti S, Ilharreborde B, Prost S, Laouissat F, et al. Variation of Global Sagittal Alignment Parameters According to Gender, Pelvic Incidence, and Age. Clin Spine Surg 2022;35:E610-20. [Crossref] [PubMed]
- Vaz G, Roussouly P, Berthonnaud E, Dimnet J. Sagittal morphology and equilibrium of pelvis and spine. Eur Spine J 2002;11:80-7. [Crossref] [PubMed]
- Schwab F, Lafage V, Boyce R, Skalli W, Farcy JP. Gravity line analysis in adult volunteers: age-related correlation with spinal parameters, pelvic parameters, and foot position. Spine (Phila Pa 1976) 2006;31:E959-67. [Crossref] [PubMed]
- Lee JH, Kim JU, Jang JS, Lee SH. Analysis of the incidence and risk factors for the progression of proximal junctional kyphosis following surgical treatment for lumbar degenerative kyphosis: minimum 2-year follow-up. Br J Neurosurg 2014;28:252-8. [Crossref] [PubMed]
- Maruo K, Ha Y, Inoue S, Samuel S, Okada E, Hu SS, Deviren V, Burch S, William S, Ames CP, Mummaneni PV, Chou D, Berven SH. Predictive factors for proximal junctional kyphosis in long fusions to the sacrum in adult spinal deformity. Spine (Phila Pa 1976) 2013;38:E1469-76. [Crossref] [PubMed]
- Horton WC, Brown CW, Bridwell KH, Glassman SD, Suk SI, Cha CW. Is there an optimal patient stance for obtaining a lateral 36" radiograph? A critical comparison of three techniques. Spine (Phila Pa 1976) 2005;30:427-33. [Crossref] [PubMed]
- Yagi M, Akilah KB, Boachie-Adjei O. Incidence, risk factors and classification of proximal junctional kyphosis: surgical outcomes review of adult idiopathic scoliosis. Spine (Phila Pa 1976) 2011;36:E60-8. [Crossref] [PubMed]
- Han SM, Wen JX, Cao L, Wu HZ, Liu C, Yang C, Yang HH, Gao BL, Wu WJ. Sagittal morphology of the cervical spine in adolescent idiopathic scoliosis: a retrospective case-control study. Quant Imaging Med Surg 2022;12:3049-60. [Crossref] [PubMed]
- Ilharreborde B, Steffen JS, Nectoux E, Vital JM, Mazda K, Skalli W, Obeid I. Angle measurement reproducibility using EOS three-dimensional reconstructions in adolescent idiopathic scoliosis treated by posterior instrumentation. Spine (Phila Pa 1976) 2011;36:E1306-13. [Crossref] [PubMed]
- Kim HJ, Bridwell KH, Lenke LG, Park MS, Song KS, Piyaskulkaew C, Chuntarapas T. Patients with proximal junctional kyphosis requiring revision surgery have higher postoperative lumbar lordosis and larger sagittal balance corrections. Spine (Phila Pa 1976) 2014;39:E576-80. [Crossref] [PubMed]
- Claeys K, Brumagne S, Deklerck J, Vanderhaeghen J, Dankaerts W. Sagittal evaluation of usual standing and sitting spinal posture. J Bodyw Mov Ther 2016;20:326-33. [Crossref] [PubMed]
- Kim JS, Phan K, Cheung ZB, Lee N, Vargas L, Arvind V, Merrill RK, Gidumal S, Di Capua J, Overley S, Dowdell J, Cho SK. Surgical, Radiographic, and Patient-Related Risk Factors for Proximal Junctional Kyphosis: A Meta-Analysis. Global Spine J 2019;9:32-40. [Crossref] [PubMed]
- Bao H, Lafage R, Liabaud B, Elysée J, Diebo BG, Poorman G, Jalai C, Passias P, Buckland A, Bess S, Errico T, Lenke LG, Gupta M, Kim HJ, Schwab F, Lafage V. Three types of sagittal alignment regarding compensation in asymptomatic adults: the contribution of the spine and lower limbs. Eur Spine J 2018;27:397-405. [Crossref] [PubMed]
- Booth KC, Bridwell KH, Lenke LG, Baldus CR, Blanke KM. Complications and predictive factors for the successful treatment of flatback deformity (fixed sagittal imbalance). Spine (Phila Pa 1976) 1999;24:1712-20. [Crossref] [PubMed]
- Glassman SD, Berven S, Bridwell K, Horton W, Dimar JR. Correlation of radiographic parameters and clinical symptoms in adult scoliosis. Spine (Phila Pa 1976) 2005;30:682-8. [Crossref] [PubMed]
- Kim YJ, Bridwell KH, Lenke LG, Rhim S, Cheh G. An analysis of sagittal spinal alignment following long adult lumbar instrumentation and fusion to L5 or S1: can we predict ideal lumbar lordosis? Spine (Phila Pa 1976) 2006;31:2343-52. [Crossref] [PubMed]
- Cerpa M, Sardar Z, Lenke L. Revision surgery in proximal junctional kyphosis. Eur Spine J 2020;29:78-85. [Crossref] [PubMed]



