Ethylene-vinyl alcohol copolymer (Onyx®) transarterial embolization for post-traumatic high-flow priapism
Introduction
Priapism is a relatively rare condition characterized by a persistent erection lasting more than 4 hours in the absence of sexual stimulation (1). There are two main subtypes: the more common ischemic, or low-flow, characterized by the impaired outflow from the corpora cavernosa, and non-ischemic, or high-flow, most often caused by trauma, characterized by the formation of arterio-cavernous fistulas and increased inflow of blood to the corpora cavernosa (1). While the painful low-flow priapism and the associated decreased oxygenation of cavernous tissue can quickly lead to a cavernous fibrosis and permanent damage to penile tissues and is, therefore, an urological emergency, high-flow priapism is often painless and can persist for months, in most cases without a permanent damage of penile tissues, but sometimes with the reduced potency. Transarterial embolization of the distal internal pudendal arteries is the treatment of choice for high-flow priapism and a useful alternative to surgery (1,2). However, the choice of embolic agent remains a debate of matter (3). Here, we report a case of high-flow priapism caused by perineal trauma that was treated successfully with superselective embolization of the cavernous artery suing ethylene-vinyl alcohol copolymer liquid agent (Onyx®). The use of Onyx® in such a setting has not been reported in the literature.
Case presentation
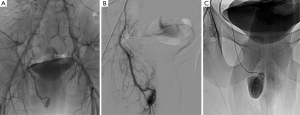
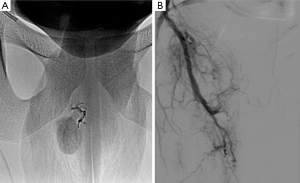
A 16-year-old man was referred from urology for possible endovascular treatment of high-flow priapism for four days. He originally presented to the urology clinic following symptoms from perineal impalement from a sports-related injury. The patient had complaints of sustained incomplete erection. Color Doppler ultrasound showed a mixed flow pattern of arterial and venous blood in the cavernosum. High-flow priapism resulting from injury to the cavernosum artery was diagnosed. Contrast-enhanced computed tomography was performed and revealed an arteriocavernosal fistula involving the right corpora cavernosa (Figure 1). Potential treatment options for this patient were endovascular embolization and conservative management. According to the American Urologic Association guidelines on the management of high-flow (nonischemic) priapism, up to 62% of cases will resolve spontaneously; however, up to one-third will have an associated complaint of erectile dysfunction (1). Given the patient’s age and desire for a rapid resolution of symptoms, endovascular embolization was chosen. By right common femoral approach, a 5-Fr catheter was placed into the right internal iliac artery. Pelvic angiography demonstrated a large arteriocavernosal fistula with intense arterial blush over the right corpora (Figure 2). Right internal pudendal arteriography confirmed an arterio-venous fistula resulting from the injury to the cavernosal artery. A 2.7-Fr microcatheter (Progreat, Terumo, Tokyo, Japan) was then superselectively advanced just beyond the site of the arteriocavernosal fistula, and embolization was carried out using 1 mL vial of ethylene-vinyl alcohol copolymer (Onyx®-18) under fluoroscopic guidance (Figure 2). A repeat angiogram revealed complete resolution of the fistula and preservation of the dorsal penile artery (Figure 3). Of note, the patient’s erection immediately detumesced following embolization. The patient was discharged 2 hours later in good condition. The morning following the procedure, he endorsed nocturnal penile tumescence. The patient was seen approximately three months following embolization and remained very pleased with the result, endorsing full erections and no further priapism.

Discussion
Priapism is defined as a persistent erection that is not induced by sexual stimulation and that lasts for more than 4 hours. The American Urological Association (AUA) guidelines include a management algorithm for priapism (1). In brief, the guidelines recommend “observation” as an initial management of non-ischemic (high-flow) priapism. Immediate invasive interventions (embolization or surgery) are recommended to be carried out at the request of the patient (2,3). In response to the patient’s request for treatment, selective arterial embolization is recommended as a second step management. Surgical management is the last option or last resort for long standing cases. In clinical practice, and although painless, arterial embolization is often performed at the patient’s request in cases of non-ischemic priapism. Although non-ischemic priapism can resolve without treatment, some authors have discussed the disadvantages of a watchful waiting strategy, including the theoretical considerations of possible structural alterations resulting from excessive arterial inflow as well as social and psychological difficulties related to the condition. Thus, if priapism does not resolve spontaneously after three weeks, highly selective embolization might be considered. Whether embolization is actually associated with a risk of erectile dysfunction is not clear. Few reports discuss about this. Savoca et al. (4) reported that patients who were treated early with embolization, most of whom were trauma patients, did not have fibrosis or changes in erectile function at the long-term follow-up examination. Transient erectile dysfunction occurs shortly after embolization in some cases. With short-term follow-up, it is difficult to determine the degree of erectile dysfunction because it may gradually improve after embolization. The time needed to improve erectile function in reported cases ranges from 7 days to 1 year. Moreover, even in cases of erectile dysfunction following embolization, it is unclear whether erectile dysfunction was caused by the embolization, prolonged priapism or perineal trauma or by conservative therapy. With recent advances in interventional radiological techniques, endovascular selective embolization of the pathological arterio-cavernous communication is firmly established as the treatment of choice in high-flow priapism (5-7). It is commonly performed using microcatheters and a range of embolization materials: gelatine sponge particles, coils or N-butyl-cyanoacrylate (8-10). Gelfoam is often preferred because of its spontaneous degradation and a reportedly lower risk of the permanent erectile dysfunction, but could have a greater recurrence rate. It should probably be used in cases of bilateral embolization. Deployment of coils can be time-consuming and not always easy to place as far as expected in very thin vessels (6). Liquid embolic agents may be very useful in such a setting. N-butyl-cyanoacrylate (Glubran®2, GEM Srl, Viareggio, Italy) and ethylene-vinyl alcohol copolymer (Onyx® LES, Covidien, Plymouth, MN, USA) provide faster and more efficient occlusion of the fistula (5). Embolization with liquid agents is permanent and carries a higher risk of ischemia of the vessel in question, and it consequently requires a better embolization technique and more experienced interventionists capable of introducing the catheter and the embolization material directly into the site of the fistula. Cyanoacrylates are probably more difficult and challenging to use given the risk of reflux into other vessels and the risk of sticking the catheter (11,12). That’s why Onyx® is very useful and safer thanks to its slow precipitation into vessels, making the procedure more predictable and controlled. The main disadvantage of Onyx® is its relatively high cost compared with other embolic agents, especially glue. In addition, chemical irritation caused by dimethyl sulfoxide (DMSO) may be painful. It is recommended to use adjuvant analgesia medication during embolization. In our case, Onyx® injection was well tolerated, without noticeable pain. In conclusion, selective arterial embolization with Onyx® is a very interesting treatment option for post-traumatic high-flow priapism. Onyx® seems to provide controlled embolization as a result of its slow polymerization, which enables deep penetration with less risk of catheter gluing because of its nonadhesive nature. We are not aware of previous reported cases of high-flow priapism treated with embolization using Onyx®.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Montague DK, Jarow J, Broderick GA, Dmochowski RR, Heaton JP, Lue TF, Nehra A, Sharlip ID. American Urological Association guideline on the management of priapism. J Urol 2003;170:1318-24. [Crossref] [PubMed]
- O'Sullivan P, Browne R, McEniff N, Lee MJ. Treatment of "high-flow" priapism with superselective transcatheter embolization: a useful alternative to surgery. Cardiovasc Intervent Radiol 2006;29:198-201. [Crossref] [PubMed]
- Abujudeh H, Mirsky D. Traumatic high-flow priapism: treatment with super-selective micro-coil embolization. Emerg Radiol 2005;11:372-4. [Crossref] [PubMed]
- Savoca G, Pietropaolo F, Scieri F, Bertolotto M, Mucelli FP, Belgrano E. Sexual function after highly selective embolization of cavernous artery in patients with high flow priapism: long-term followup. J Urol 2004;172:644-7. [Crossref] [PubMed]
- Rados M, Sunjara V, Sjekavica I, Padovan RS. Post-traumatic high-flow priapism treated by endovascular embolization using N-butyl-cyanoacrylate. Radiol Oncol 2010;44:103-6. [Crossref] [PubMed]
- Chadha DS, Sivaramakrishna B, Rastogi V. Microcoil embolization in post-traumatic high-flow priapism. J Invasive Cardiol 2011;23:E147-9. [PubMed]
- Tan ZY, Burnes J. Post-traumatic pre-pubertal high-flow priapism: bilateral superselective embolisation. J Med Imaging Radiat Oncol 2011;55:498-501. [Crossref] [PubMed]
- Touge H, Watanabe T, Fujinaga T, Kawabata M. Post-traumatic high flow priapism: a case report. Int J Urol 1999;6:623-6. [Crossref] [PubMed]
- Corbetta JP, Durán V, Burek C, Sager C, Weller S, Paz E, Lopez JC. High flow priapism: diagnosis and treatment in pediatric population. Pediatr Surg Int 2011;27:1217-21. [Crossref] [PubMed]
- Pieri S, Agresti P, La Pera G, Atzori M, Ialongo P. Post-traumatic high flow priapism percutaneously treated with transcatheter embolisation. Radiol Med 2005;110:370-7. [PubMed]
- Loffroy R, Guiu B, Cercueil JP, Krausé D. Endovascular therapeutic embolisation: an overview of occluding agents and their effects on embolised tissues. Curr Vasc Pharmacol 2009;7:250-63. [Crossref] [PubMed]
- Favard N, Moulin M, Fauque P, Bertaut A, Favelier S, Estivalet L, Michel F, Cormier L, Sagot P, Loffroy R. Comparison of three different embolic materials for varicocele embolization: retrospective study of tolerance, radiation and recurrence rate. Quant Imaging Med Surg 2015;5:806-14. [PubMed]


