
Multimodal imaging findings in a patient with bilateral panuveitis secondary to Mycoplasma pneumoniae infection
Herein, we report multimodal imaging findings of a Chinese child with bilateral panuveitis secondary to Mycoplasma pneumoniae (M. pneumoniae) infection. M. pneumoniae belongs to a class of Mollicutes bacterium, and commonly causes atypical pneumonia in children and young adults. The main feature of mycoplasma infection is a respiratory disease with extrapulmonary manifestations occurring in up to 25% of infected patients. M. pneumoniae has been reported to cause ocular disease, with conjunctivitis being the most common outcome; cranial neuropathy, optic nerve papillitis, and anterior uveitis are rare outcomes (1).
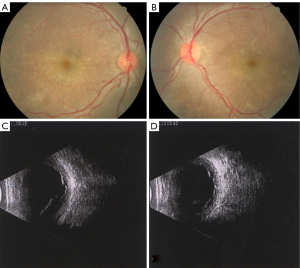
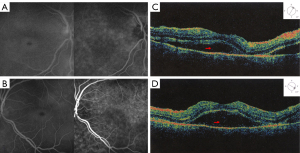
We investigated fundus characteristics of M. pneumoniae uveitis in an 8-year-old boy using fundus photography, optical coherence tomography (OCT), fluorescein angiography (FA), and indocyanine green angiography (ICGA). The patient complained of blurred vision in both eyes for 3 days, without ophthalmodynia, black shadows, distortion, double vision, alopecia, vitiligo, nausea, or vomiting. He reported fever for 8 days prior to the onset of symptoms. The patient’s visual acuity was 20/500 for the right eye and 20/500 for the left eye. Aqueous flares and 5-mm dilated pupils without both direct and consensual light reflexes were noted in both eyes. Fundus examination revealed vitreous opacity, optic disc hyperaemia, exudative retinal detachment, and white sheath of retinal vessels. Ocular B ultrasound revealed bilateral exudative retinal detachments (Figure 1). OCT revealed serous macular detachment in both eyes. FA and ICGA revealed microvascular dilatation and leakage in the retina and choroid without obvious staining of the optic discs in both eyes (Figure 2). Laboratory tests were positive for M. pneumoniae antibody (1:160), M. pneumoniae serum test (IgM), and mycoplasma inflammatory serum test (IgG). Lung computed tomography (CT) revealed bilateral pneumonia. However, the craniocerebral CT findings, intracranial pressure, and immune status were normal. The patient was diagnosed with bilateral panuveitis secondary to M. pneumoniae infection and was referred for paediatric treatment. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
The serum of patients with mycoplasma-associated pneumonia contains circulating immune complexes that cause type III hypersensitivity reactions and can deposit along the blood vessel walls of the eye causing microvasculitis. Immune complexes can also alter the blood supply to the optic nerve head, resulting in swelling of the nerve head. In patients with mycoplasma infection, uveitis can also be caused by direct bacterial invasion (1).
Cases of bilateral optic disc oedema, optic neuritis, and/or uveitis following M. pneumoniae infection have been reported (2). The extrapulmonary manifestations of mycoplasma pneumonia may occur in any organ system. Except for conjunctivitis, ocular manifestations of M. pneumoniae infection are uncommon. However, in our case, fundus examination revealed vitreous opacity, optic disc hyperaemia, exudative retinal detachment, white sheath of retinal vessels, and a small patchy haemorrhage. Matsou et al. reported bilateral intermediate uveitis with the appearance of frosted branch angiitis associated with M. pneumoniae infection (3). Optic disc swelling, optic nerve atrophy, retinal exudation and haemorrhage, and cranial nerve palsy have rarely been reported (4). Central nervous system complications, including encephalitis, meningitis, papilloedema, and papillitis, are estimated to occur in 0.1% of cases (5). However, in this case, optic disc hyperaemia, and bilateral disc enlargement occurred without elevation of intracranial pressure, which differed from the findings in previous studies (4,5). Most cases reported in the literature show vision recovery to some extent after resolution of the optic disc hyperaemia (6).
The limitation of this study was that we did not test intraocular fluid for the presence of M. pneumoniae antibodies. Nevertheless, to the best of our knowledge, this is the first report of multimodal imaging findings of bilateral panuveitis secondary to M. pneumoniae infection in a Chinese patient. Our findings may be beneficial for both diagnosis and treatment of ocular complications of M. pneumoniae infection.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://qims.amegroups.com/article/view/10.21037/qims-22-455/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Liu EM, Janigian RH. Mycoplasma pneumoniae: the other masquerader. JAMA Ophthalmol 2013;131:251-3. [Crossref] [PubMed]
- Perry JT, Chen WS. Acute Mycoplasma pneumoniae infection presenting with unilateral anterior uveitis and perineuritis. J AAPOS 2016;20:178-80. [Crossref] [PubMed]
- Matsou A, Riga P, Samouilidou M, Dimitrakos S, Anastasopoulos E. Bilateral intermediate uveitis with appearance of frosted branch angiitis and association with Mycoplasma pneumoniae infection: case report and review of the literature. J AAPOS 2016;20:358-61. [Crossref] [PubMed]
- Salzman MB, Sood SK, Slavin ML, Rubin LG. Ocular manifestations of Mycoplasma pneumoniae infection. Clin Infect Dis 1992;14:1137-9. [Crossref] [PubMed]
- Yip IYM, Scotcher S. Raised intracranial pressure with bilateral anterior uveitis. BMJ Case Rep 2018;2018:bcr2017222504. [Crossref] [PubMed]
- Milla E, Zografos L, Piguet B. Bilateral optic papillitis following mycoplasma pneumoniae pneumonia. Ophthalmologica 1998;212:344-6. [Crossref] [PubMed]


