
Contrast-enhanced ultrasound-based Bosniak classification for evaluating of a cystic renal mass: a rare case description of renal hemolymphangioma
Introduction
Hemolymphangioma is a very rare benign tumor. Couinaud et al. (1) in 1966 reported the first case of hemolymphangioma, which was located in the pancreas. Patients with hemolymphangioma often do not have any specific clinical manifestations, and are incidentally diagnosed during physical examination. Complete surgical resection is the preferred treatment for hemolymphangioma, which has a good prognosis post- operation, so preoperative diagnosis is essential. At present, the preoperative examination of hemolymphangioma mainly depends on imaging examination (2,3). In general, the tumor presents as a large cystic mass with multiple septa. The Bosniak classification is widely used to stratify the risk of malignancy in cystic renal masses. This computerized tomography (CT)-based classification is useful in clinical practice and was modified by Silverman et al. in 2019 (Bosniak Classification, version 2019) (4). The emergence of ultrasound contrast agents (UCA) makes it possible to characterize cystic renal masses by contrast-enhanced ultrasound (CEUS). However, the efficacy of CEUS to classify cystic renal masses remains controversial (5-7) and there has not yet been a guideline on CEUS-based Bosniak classification. EFSUMB Expert Task Force published a position statement in 2020 (8) to provide proposal for CEUS-based Bosniak cyst categorization. Herein, we reported a case of Bosniak III as per CEUS-based Bosniak classification, with a pathological diagnosis of renal hemolymphangioma. We also reviewed the relevant literature to improve the understanding of renal hemolymphangioma and explore the pros and cons of CEUS-based Bosniak classification versus CT-based Bosniak classification.
Case presentation
A 68-year-old male patient with hypertension for 20 years was admitted to our hospital due to lumbodynia of unknown etiology for the past two months. Polyuria, urgency of urination, and urodynia were absent. The patient denied history of trauma or surgery. No abnormalities were found in the physical examination. Laboratory examination revealed no abnormalities of the liver, renal function, blood, or urine analysis. The patient received imaging examinations.
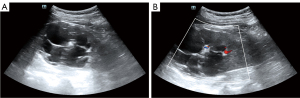
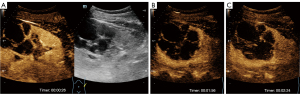
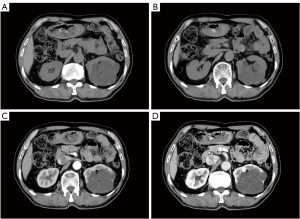
First, the patient underwent an ultrasound examination of the urinary system by a Resona7 ultrasound system (Mindray, China) equipped with an SC6-1U (1–6 MHz) transducer. The grayscale ultrasound image demonstrated a multi-locular cystic mass with multiple septa (≥6) and calcification in the upper part of the left kidney. The mass was approximately 9.1 cm × 6.4 cm, with an irregular shape and sharp margins (Figure 1A). Color Doppler flow imaging (CDFI) displayed dot-linear blood flow signals in some septa (Figure 1B). In CEUS, the parameters of the machine, including depth, gain, and focus, were thoroughly adjusted for the optimal display according to the operator’s experience. During the whole process of CEUS, the mechanical index setting was 0.078. Meanwhile, 1.2 mL UCA SonoVue (Bracco, Milan, Italy) suspension was injected through the patient’s cubital vein followed by 5 mL saline flush. The timer was started when the contrast agent injection was completed. Taking the normal renal parenchyma as a reference, the SonoVue reached the mass in 14 seconds after administration, and the wall and septa of the mass showed homogeneous mild hyper-enhancement in the cortical phase (Figure 2A). The mass had many uneven thickened septa (the thickest septum was approximately 6 mm) without obvious wall nodules. In the parenchymal phase, the wall and septa displayed hypo-enhancement (Figure 2B,2C). No enhancing solid components were observed during CEUS. According to CEUS-adapted Bosniak classification (5), the mass was classified as Bosniak III. Then, CT examination was performed with a uCT780 scanner (UNITED IMAGING, China), with injection of the contrast agent iohexol (300 mg/mL, dose 1.5 mL/kg). Unenhanced CT revealed 8.7 cm × 6.3 cm low density mass within multiple linear slightly high-density shadows and patchy calcification in the left kidney (Figure 3A,3B). Contrast-enhanced CT (CECT) demonstrated a few thickened (≥3 mm) continuous enhancement septa during the nephrographic phase of the mass. Meanwhile, most areas of the mass displayed no enhancement during the whole scan (Figure 3C,3D). According to Bosniak classification, version 2019 (4), the mass was classified as Bosniak IIF.
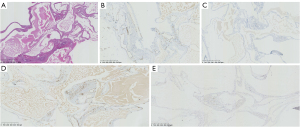
Thereafter, the patient underwent left nephrectomy to remove the mass. Macroscopically, the mass measured 9.0 cm × 8.0 cm × 7.0 cm. Microscopic examination showed that the tumor consisted of lymphatic and blood vessels (Figure 4A). Immunohistochemistry revealed positive expression of CD31, CD3, D2-40, and ERG (Figure 4B-4E). Based on the morphological and immunohistochemical analyses, the final pathological diagnosis of the mass was a renal hemolymphangioma. No evidence of malignancy was found. The patient had rapid postoperative recovery and was subsequently discharged with recovery from the hospital after 12 days. To date, the patient has been following-up for 2 years, and no abnormalities were found in regular imaging examinations every 6 months.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
Hemolymphangioma is an extremely rare, benign tumor originating from mesenchymal tissue, which may be caused by the developmental defects or abnormalities in angiogenesis and lymphangiogenesis. The tumor consists of abnormal lymphatic and blood vessels with polycystic spaces (9), and is usually found in the head, axilla, and neck. Although it is considered a benign neoplasm, hemolymphangioma can invade surrounding organs and recur after treatment (10-12). Surgical resection is often the main treatment, although it can recur after surgery. The recurrence rate after complete resection of the lesion is 10–27%, and the recurrence rate after partial resection is 50–100% (13). In general, hemolymphangioma presents as a large cystic mass with various-sized cavities and thin walls. Some reports (14,15) indicated that the tumor size varies due to the anatomical location and relationship with the neighboring tissues. Hemolymphangioma has historically demonstrated a female predilection (2.25:1 female to male) and presentation in the third to fourth decades of life (11). A literature review indicated that that the clinical symptoms were nonspecific, and atypical abdominal pain or compression discomfort of nearby anatomic structures was the primary reported manifestation (16).
Hemolymphangioma often presents as a well-defined multi-ocular cystic mass on imaging (2,13). However, these appearances are similar to some complex renal cystic masses, such as lymphangioma. Lymphangioma can occur in any part of the body, usually due to congenital abnormal development of lymphatic vessels, pathologically manifesting as lymphatic structures. It is challenging for any imaging modality to accurately differentiate the two types of tumors. The final diagnosis is based on a combination of clinical, radiological, and histopathological findings. D2-40 is a marker of lymphatic endothelium, which is strongly expressed in lymphatic endothelium, but not in blood vessel endothelial cells (17). CD31 is regarded as the most sensitive and specific immunohistochemical marker for the detection of endothelial differentiation. CD34 is strongly expressed in hemangiomas and other vascular tumors (18). Positive expression of D2-40 and CD31/CD34 can provide an important basis for the diagnosis of hemolymphangioma.
In the latest 2019 version (4), cystic renal masses were divided into five Bosniak grades I, II, IIF, III, and IV, based on the characteristic manifestations of CT or MRI examination, such as the density value, the presence or absence of septa in cystic masses, the thickness of wall and septa, whether wall and septa was enhanced. Given the higher temporal and spatial resolution of CEUS compared to CECT, CEUS-based Bosniak classification (8) was developed on the basis of CT-Bosniak according to the CEUS findings. Comparison of CEUS-based Bosniak and CT-Bosniak in the present case indicated that CECT showed only a small number of thin septa, so the mass was classified as Bosniak IIF. However, although the mass had no wall nodules, multiple septa and thickened septa with hyper-enhancement were important malignant signs of the CEUS-based Bosniak classification, so the mass was classified as Bosniak III. After analyzing the reasons for the different classes of the two imaging modalities, we speculated that as a pure blood pool contrast agent, CEUS has high temporal and spatial resolution, and is more sensitive to the septa of cystic masses and the microperfusion of walls and septa (19,20). The dose of contrast injected may also affect the results. If an excessive dose of UCA is injected (microbubble piling and blooming artifact), thin septa with weak enhancement can present as thicker septa with heavy enhancement (8). Our study has limitations mainly related to the CEUS-based Bosniak classification used in this article. There has not yet been a guideline on CEUS-based Bosniak classification. The CEUS-based Bosniak classification used in this article is a proposal and evaluation efficiency needs further validation, which may affect the result. In addition, the CEUS-based Bosniak classification is intrinsically subjective and based on the observer’s experience in CEUS interpretation. These factors may cause the CEUS-based Bosniak classification to upgrade the risk of malignancy of renal cystic masses. According to the literature reports, the accuracy of CEUS-based Bosniak classification in the diagnosis of renal cystic malignant masses is higher than that of CT-Bosniak classification. However, 31% of renal cysts were attributed to a higher Bosniak category compared to CECT (21-25). In the present case, we speculated that based on the Bosniak III class (a roughly 50% risk of malignancy) and imaging experience [a substantial proportion of malignant complex cystic masses represent cystic renal cell carcinoma (26)], the mass was further considered malignant and as cystic renal cell carcinoma by the ultrasound physician. The result indicated CECT has good performance in the diagnosis of cystic renal mass. These findings suggested that CEUS-based Bosniak classification needs to be continuously improved in clinical application to reach a consensus of high diagnostic value.
Conclusions
Herein, we reported a rare renal hemolymphangioma, which appeared as a large, complex cystic mass on imaging and was classified as different class by CT-based Bosniak classification, version 2019 and CEUS-based Bosniak classification. For better specificity and reporting standardization in the categorization of renal cystic masses, CEUS-based Bosniak classification needs to be improved, based on the unique characteristics of the CEUS examination. Although renal hemolymphangioma is often difficult to diagnose due to its low incidence, nonspecific clinical and imaging features, it is necessary for doctors to further accumulate experience and make a comprehensive judgment in combination with other clinical data and imaging findings to improve diagnosis, treatment, and outcomes.
Acknowledgments
This manuscript has been released as a preprint at Research Square source (Wang H, Yang D, Luo Y, Peng YL, Ling WW. Contrast-enhanced Ultrasound Findings of Hemolymphangioma of the Kidney: The First Report in the Literature, Research Square, 2020. DOI:10.21203/rs.3.rs-54604/v1).
Funding: This research was supported by a grant from the Sichuan Science and Technology Program (No. 2020YFS0211).
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://qims.amegroups.com/article/view/10.21037/qims-22-518/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Couinaud J, Prot C. Hemolymphangioma of the head of the pancreas. Mem Acad Chir (Paris) 1966;92:152-5. [PubMed]
- Dong F, Zheng Y, Wu JJ, Fu YB, Jin K, Chao M. Hemolymphangioma: a rare differential diagnosis of cystic-solid or cystic tumors of the pancreas. World J Gastroenterol 2013;19:3520-3. [Crossref] [PubMed]
- Hu HJ, Jing QY, Li FY. Hepatic Hemolymphangioma Manifesting as Severe Anemia. J Gastrointest Surg 2018;22:548-9. [Crossref] [PubMed]
- Silverman SG, Pedrosa I, Ellis JH, Hindman NM, Schieda N, Smith AD, Remer EM, Shinagare AB, Curci NE, Raman SS, Wells SA, Kaffenberger SD, Wang ZJ, Chandarana H, Davenport MS. Bosniak Classification of Cystic Renal Masses, Version 2019: An Update Proposal and Needs Assessment. Radiology 2019;292:475-88. [Crossref] [PubMed]
- Lee CH, Liu JJK, Zheng Y, Tan CH. Bosniak classification of cystic renal masses: utility of contrastenhanced ultrasound using version 2019. Med Ultrason 2020;22:279-86. [Crossref] [PubMed]
- Sanz E, Hevia V, Gómez V, Álvarez S, Fabuel JJ, Martínez L, Rodriguez-Patrón R, González-Gordaliza C, Burgos FJ. Renal Complex Cystic Masses: Usefulness of Contrast-Enhanced Ultrasound (CEUS) in Their Assessment and Its Agreement with Computed Tomography. Curr Urol Rep 2016;17:89. [Crossref] [PubMed]
- Angelini L, Gioulis E, Civitareale N, et al. Assessment of Contrast-Enhanced Ultrasound (CEUS) and Computed Tomography (CT) diagnostic accuracy in the evaluation of challenging cystic renal masses. J Ultrasound 2022; Epub ahead of print. [Crossref] [PubMed]
- Cantisani V, Bertolotto M, Clevert DA, Correas JM, Drudi FM, Fischer T, Gilja OH, Granata A, Graumann O, Harvey CJ, Ignee A, Jenssen C, Lerchbaumer MH, Ragel M, Saftoiu A, Serra AL, Stock KF, Webb J, Sidhu PS. EFSUMB 2020 Proposal for a Contrast-Enhanced Ultrasound-Adapted Bosniak Cyst Categorization - Position Statement. Ultraschall Med 2021;42:154-66. [Crossref] [PubMed]
- Sun LF, Ye HL, Zhou QY, Ding KF, Qiu PL, Deng YC, Zhang SZ, Zheng S. A giant hemolymphangioma of the pancreas in a 20-year-old girl: a report of one case and review of the literature. World J Surg Oncol 2009;7:31. [Crossref] [PubMed]
- Chen G, Cui W, Ji XQ, Du JF. Diffuse hemolymphangioma of the rectum: a report of a rare case. World J Gastroenterol 2013;19:1494-7. [Crossref] [PubMed]
- Kim WT, Lee SW, Lee JU. Bleeding gastric hemolymphangioma: endoscopic therapy is feasible. Dig Endosc 2013;25:553-4. [Crossref] [PubMed]
- Li Y, Pang X, Yang H, Gao C, Peng B. Hemolymphangioma of the waist: A case report and review of the literature. Oncol Lett 2015;9:2629-32. [Crossref] [PubMed]
- Zhang X, Sheng X, Liu F, Jian R, Li L, Luo R. Hemolymphangioma of the chest wall: A rare case report. Oncol Lett 2012;3:816-8. [PubMed]
- Li Y, Zhang X, Pang X, Yang L, Peng B. Occipitocervical Hemolymphangioma in an Adult with Neck Pain and Stiffness: Case Report and Literature Review. Case Rep Med 2017;2017:7317289. [Crossref] [PubMed]
- Swarup I, Bjerke-Kroll BT, Cunningham ME. Paraspinous hemolymphangioma associated with adolescent scoliosis. World J Clin Cases 2015;3:514-8. [Crossref] [PubMed]
- Toyoki Y, Hakamada K, Narumi S, Nara M, Kudoh D, Ishido K, Sasaki M. A case of invasive hemolymphangioma of the pancreas. World J Gastroenterol 2008;14:2932-4. [Crossref] [PubMed]
- Kalof AN, Cooper K. D2-40 immunohistochemistry--so far! Adv Anat Pathol 2009;16:62-4. [Crossref] [PubMed]
- Ordóñez NG. Immunohistochemical endothelial markers: a review. Adv Anat Pathol 2012;19:281-95. [Crossref] [PubMed]
- Rübenthaler J, Mueller-Peltzer K, Negrão de Figueiredo G, Gresser E, Clevert DA. CEUS-diagnostic workup of cystic renal lesions. Radiologe 2018;58:545-52. [PubMed]
- Wei S, Tian F, Xia Q, Huang P, Zhang Y, Xia Z, Wu M, Yang B. Contrast-enhanced ultrasound findings of adult renal cell carcinoma associated with Xp11.2 translocation/TFE3 gene fusion: comparison with clear cell renal cell carcinoma and papillary renal cell carcinoma. Cancer Imaging 2019;20:1. [Crossref] [PubMed]
- Ascenti G, Mazziotti S, Zimbaro G, Settineri N, Magno C, Melloni D, Caruso R, Scribano E. Complex cystic renal masses: characterization with contrast-enhanced US. Radiology 2007;243:158-65. [Crossref] [PubMed]
- Quaia E, Bertolotto M, Cioffi V, Rossi A, Baratella E, Pizzolato R, Cov MA. Comparison of contrast-enhanced sonography with unenhanced sonography and contrast-enhanced CT in the diagnosis of malignancy in complex cystic renal masses. AJR Am J Roentgenol 2008;191:1239-49. [Crossref] [PubMed]
- Robbin ML, Lockhart ME, Barr RG. Renal imaging with ultrasound contrast: current status. Radiol Clin North Am 2003;41:963-78. [Crossref] [PubMed]
- Park BK, Kim B, Kim SH, Ko K, Lee HM, Choi HY. Assessment of cystic renal masses based on Bosniak classification: comparison of CT and contrast-enhanced US. Eur J Radiol 2007;61:310-4. [Crossref] [PubMed]
- Ragel M, Nedumaran A, Makowska-Webb J. Prospective comparison of use of contrast-enhanced ultrasound and contrast-enhanced computed tomography in the Bosniak classification of complex renal cysts. Ultrasound 2016;24:6-16. [Crossref] [PubMed]
- Donin NM, Mohan S, Pham H, Chandarana H, Doshi A, Deng FM, Stifelman MD, Taneja SS, Huang WC. Clinicopathologic outcomes of cystic renal cell carcinoma. Clin Genitourin Cancer 2015;13:67-70. [Crossref] [PubMed]


