
Axial loading lumbar magnetic resonance imaging with a new device in asymptomatic individuals
Introduction
Magnetic resonance imaging (MRI) is currently the best non-invasive examination for the diagnosis of lumbar spine disorders, because it has excellent soft tissue contrast and provides good visualization of anatomical structures (1-3). A conventional lumbar MRI examination is usually performed in the supine position with no load on the lumbar spine, which fails to reflect the real conditions of the lumbar spine in the upright position, resulting in the discrepancy between imaging and clinical symptoms (4-8).
To solve this problem, the axial loading MRI technology has been developed to simulate the pathological changes of the lumbar spine in the upright position. Until now, several clinical studies have confirmed that axial loading MRI could improve the accuracy of the diagnosis of lumbar spinal stenosis thus change the clinical treatment strategy (9-12). Currently, the only device for axial loading MRI is the DynaWell L-Spine (DynaWell Diagnostics, NY, USA), which has some defects, including instability in exerting force, complex operation, and high cost (13,14). In an effort to address these deficiencies, we developed a new lumbar axial loading device. The present study aimed to investigate the effect and examinee comfort of this new device for axial loading lumbar MRI in asymptomatic volunteers.
Methods
Patients
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the Institutional Review Board of the 305 Hospital of PLA, Beijing, and informed consent was obtained from all the participants. Thirty asymptomatic volunteers, with an average age of 35.3 years, were included in the study. None of the participants had any history of low back pain or sciatica. The exclusion criteria included previous spinal surgery, severe osteoporosis, severe cardiopulmonary dysfunction, a history of spinal fracture, spinal malignant tumor, lower limb disease, and claustrophobia.
Axial loading device
The new lumbar axial loading MRI device consists of wearable components and pressure components, which achieve lumbar loading by exerting pressure on the shoulders and hips. The pressure is applied in the pneumatic mode. Through the inflation of the control system, air is transmitted from the vent pipe to the cylinder, and the connecting belt is tightened after the cylinder is pressurized, which allows the pressure to be applied stably and measured accurately (Figure 1).

The volunteers laid on the examination bed with the wearable components and then the pressure was applied. The pressure adjustment knob was used to control the strength at 40–50% of the body weight, simulating the load weight of the lumbar when the body is upright, and the compression time was 5 minutes (12,15,16). Then, axial loading MRI scanning of the lumbar was performed. During the examination, a small cushion was placed underneath the lumbar spine to achieve lordosis, simulating the upright position.
Imaging technique
All MRI examinations were performed on a 1.5-T system (Signa Optima, GE Medical Systems, Milwaukee, WI, USA) using a surface coil. Sagittal T2-weighted fast recovery fast spin-echo (FRFSE), T1-weighted fast spin-echo (FSE), and axial T2-weighted FRFSE sequences were performed. The repetition time/echo time (TR/TE) was 450–525/9–16 for T1-weighted images and 2,600–3,800/110–130 for T2-weighted images. The field of view (FOV) was 320×320 for sagittal images and 200×200 for axial images, and the slice thickness was 4 mm. The imaging matrix was 320×256 for sagittal images and 320×220 for axial images.
All the participants first underwent conventional MRI scanning, followed by axial loading MRI scanning. All MRI examinations were performed between 6:00 pm and 9:00 pm to exclude the effects of diurnal variations on the lumbar spine.
Image interpretation and measurement
Two experienced radiologists analyzed the images using a workstation (AW, version 4.6, GE Medical Systems). The MRI images were sent to the radiologists with all participant information withheld. The radiologists were also blinded to whether the images had been obtained with or without axial loading. The dural sac cross-sectional area (DSCA), sagittal vertebral canal diameter (SVCD), and disc height (DH) were measured at L3-4, L4-5, and L5-S1. The SVCD, which was the distance from the midpoint of the posterior edge of the intervertebral disc to the base of the spinous process, was measured in the transverse axial image. The DH was averaged from the anterior edge, midline, and posterior edge of the intervertebral space. Three measurements were performed for each disc space and the values were averaged.
Examinee comfort assessment
After undergoing axial loading MRI, the participants were asked to assess the level of comfort of the two examinations on a 5-point scale, as follows: 1 point, no discomfort during the examination; 2 points, only mild discomfort during the examination; 3 points, certain discomfort but the MRI could be undertaken with ease; 4 points, obvious discomfort but the MRI could be completed; and 5 points, intolerable discomfort and the MRI could not be performed.
Statistical analysis
The statistical analyses were performed using the SPSS 25.0 software (IBM Corp., Armonk, NY, USA). The cohort was characterized using means and standard deviations to describe continuous variables and proportions to describe categorical variables. Unadjusted bivariate analyses were conducted using paired t-tests for continuous variables. Examinee comfort was compared between the two examinations using the Wilcoxon signed-rank test. Statistical significance was defined as P<0.05. For comparison between the supine and standing positions, a P value with two tails was reported. Inter-observer reproducibility and intra-observer reproducibility for the quantitative radiological measurements were calculated using the intraclass correlation coefficient (ICC) (17). Absolute agreement, two-way random effects, and single-measure models were adopted. Poor, moderate, good, and excellent agreement was represented by ICC values of less than 0.4, between 0.4 and 0.74, between 0.75 and 0.9, and exceeding 0.9, respectively.
Results
Study population
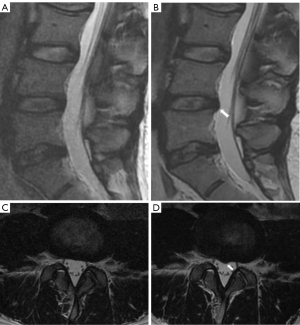
All 30 asymptomatic volunteers (15 males and 15 females) completed their examinations successfully, and the image quality was satisfactory. The baseline characteristics of the study participants and obvious changes in the intervertebral disc are summarized in Table 1. After axial loading, three intervertebral disc levels of three volunteers had definite imaging-diagnosable disc herniation or bulging, despite having no relevant clinical symptoms (Figure 2).
Table 1
| Baseline characteristics | Male (n=15) | Female (n=15) |
|---|---|---|
| Age(years)a | 34±16 | 38±14 |
| Height (cm)a | 177.1±6.0 | 163.5±6.9 |
| Body weight (kg)a | 76.6±9.8 | 59.6±6.8 |
| Body mass index (kg/m2)a | 24.4±2.7 | 22.3±2.8 |
| Disc herniation or bulging | ||
| L3-4 | – | – |
| L4-5 | 1 | 1 |
| L5-S1 | 1 | – |
a, values are presented as mean ± standard deviation.
Measurements
The mean DSCA, SVCD, and DH values for all the volunteers at each level tested are listed in Table 2. The DSCA and SVCD at the L4-5 level demonstrated a statistically significant difference after axial loading (P<0.05; Table 2). The DSCA, SVCD, and DH all showed the greatest reduction after axial loading at the L4-5 level, with declines of 7.7%, 4.6%, and 2.7%, respectively, followed by L5-S1, with decreases of 6.0%, 3.5%, and 2.4%, respectively, and L3-4, with decreases of 3.6%, 4.1%, and 1.9%, respectively.
Table 2
| Variables | Conventional MRI | Axial loading MRI | Difference (%) | P value |
|---|---|---|---|---|
| DSCA (mm2)a | ||||
| L3-4 | 154.18±18.33 | 148.64±20.11 | 5.54±4.02 (3.6) | 0.274 |
| L4-5 | 136.18±16.24 | 125.64±19.06 | 10.54±9.15 (7.7) | 0.026* |
| L5-S1 | 128.06±15.22 | 120.35±17.17 | 7.71±6.86 (6.0) | 0.074 |
| SVCD (mm)a | ||||
| L3-4 | 22.89±2.90 | 21.93±1.78 | 0.96±0.74 (4.1) | 0.129 |
| L4-5 | 17.78±1.66 | 16.96±1.32 | 0.82±1.22 (4.6) | 0.039* |
| L5-S1 | 16.45±1.27 | 15.87±1.16 | 0.58±0.83 (3.5) | 0.070 |
| DH (mm)a | ||||
| L3-4 | 10.63±0.73 | 10.44±0.64 | 0.19±0.33 (1.9) | 0.288 |
| L4-5 | 11.49±0.72 | 11.18±0.65 | 0.31±0.39 (2.7) | 0.085 |
| L5-S1 | 11.46±0.71 | 11.19±0.69 | 0.27±0.45 (2.4) | 0.141 |
a, values are presented as mean ± SD; *, P<0.05. DSCA, dural sac cross-sectional area; SVCD, sagittal vertebral canal diameter; DH, disc height; MRI, magnetic resonance imaging; SD, standard deviation.
Comfort assessment
During the two examinations, no difference in comfort level was reported by the examinees (P=0.83; Table 3). Upon questioning, the discomfort of the three high scorers (one with a score of 4 and two with a score of 3) was found to be due to experiences of panic and chest tightness in response to having their heads placed within a magnetic body.
Table 3
| Score | Conventional MRI | Axial loading MRI |
|---|---|---|
| 1 | 14 | 11 |
| 2 | 13 | 16 |
| 3 | 2 | 2 |
| 4 | 1 | 1 |
| 5 | – | – |
1= no discomfort; 2= mild discomfort; 3= certain discomfort but MRI can be done easily; 4= obvious discomfort but MRI can be done persistently; 5= intolerable discomfort and MRI cannot be done. MRI, magnetic resonance imaging.
Inter- and intra-observer reliability
The inter-observer ICCs for the DSCA, SVCD, and DH were 0.995, 0.994, and 0.873, respectively, suggesting good to excellent reliability. The intra-observer ICCs for the above measurements were 0.921, 0.972, and 0.953, respectively, suggesting excellent reliability.
Discussion
Previous studies have confirmed that lumbar axial loading MRI plays an important role in the diagnosis of lumbar diseases. The DynaWell L-Spine currently used in clinic achieves lumbar loading by exerting pressure on the shoulders and feet. However, the pressure may vary during the examination due to mild movement of the hip and knee joints, such as slight flexion of the knees. Furthermore, the device uses a manual rotating knob to adjust the tension of the connecting belt mechanically. If the patient is uncomfortable or needs to readjust the pressure during the examination process, the technician is required to return to their bedside to assist (13,14,18-21).
The new device we have developed exerts pressure on the shoulders and hips, which prevents the occurrence of pressure changes due to movement of the knee or hip joint, thus improving the stability of the pressure on the lumbar spine. In the aspect of pressure regulation, we have innovatively adopted the pneumatic mode, which can be perfectly applied to the magnetic field and ensure the stability and accurate measurement of the required pressure applied. The vent pipe connected to the control system is directed through a ground slot to the operation room, where pressurization can be controlled. If conditions do not permit, the control system can be placed as far away from the magnet as possible in the magnet room.
This study recruited 30 asymptomatic volunteers instead of patients with symptoms. Since our device is unprecedented, we needed to study whether it could successfully complete the examination without causing obvious discomfort to the examinee. More importantly, we wanted to determine whether the device could meet the needs of axial load. The test results showed that the device met the requirements in both aspects.
All 30 volunteers completed their examinations successfully, with satisfactory image quality. In the comfort assessment, the volunteers reported experiencing discomfort caused by the MRI, such as discomfort from having their head within a magnetic body, more than discomfort caused by pressure. Two male volunteers reported perineal compression discomfort, and in subsequent device improvements, we added cushions to the perineal wearing components to reduce compression.
The DSCA, SVCD, and DH are the most commonly used parameters for evaluating changes in lumbar vertebrae after loading, and can most directly reflect the changes in the intervertebral disc and the structure of the spinal canal (22-24). In our study, in most participants, the DSCA, SVCD, and DH at three disc levels changed to a certain extent after axial loading, and the DSCA and SVCD at L4-5 decreased statistically significantly. Some studies have also reported slight changes in the lumbar angle after loading (25,26). A study of asymptomatic individuals using the DynaWell device found that the decrease of DSCA in L4-5 was the most significant, but no other related data, such as SVCD and DH, were measured (27). They also found cases of imaging-diagnosable disc herniation or bulging after lumbar loading in individuals with no clinical symptoms. There were three such cases in our study, which indicates the need to combine clinical symptoms, signs, and imaging findings for the diagnosis of lumbar intervertebral disc herniation.
Axial loading MRI is of great significance. It is the only method that can simulate the stress of the lumbar spine in combination with conventional MRI. Another method is upright MRI, which can truly reflect the pathological changes of the patients under lumbar loading. It is also suitable for studying lumbar changes in complex positions, such as hyperextension and flexion spinal rotation. However, this kind of examination needs to be equipped with special upright MRI equipment, which is expensive, and the magnetic field strength is low (0.25–0.6 T), so the image quality is relatively poor (28-32).
The discussion on whether the axial loading MRI is the same as the upright MRI is of little significance. The state of the lumbar is not fixed when people are upright, and the lumbar also changes dynamically with the extension of upright time and walking distance (33). Moreover, during upright MRI examination, examinees are instructed to lean slightly backward against the examination bench and to rest their arms at a crossing bar to hold, which is still different from the normal upright position (34). Kanno et al. (35) studied the relationship between axial stress MRI and orthostatic myelography. Their results showed a significant positive correlation between the significant reduction in the DSCA in the two examinations. Axial loading MRI could reflect the changes in the DSCA during upright myelography in patients with lumbar spinal stenosis, which has higher sensitivity and specificity than conventional MRI. Some studies have shown that through the use of axial loading MRI, the diagnoses of some patients with spinal stenosis could be confirmed, and the treatment strategy changed from conservative treatment to surgical treatment (9,36). Therefore, the significance of lumbar axial loading MRI is that it can make the clinical symptoms of patients conform to the imaging findings and enable clear diagnoses of patients that can further influence clinical decision-making. Mahato et al. (37) used upright plus axial loading MRI concurrently. The manifestations of spinal canal stenosis and spondylolisthesis were obvious, representing an increase in the sensitivity of the examination, which might have a noticeable impact on clinical decision-making.
Our study had some limitations. Although we designed and developed a new device and verified its practicability through preliminary experiments, our findings are currently limited to healthy asymptomatic volunteers, and the results might not be easily applied to clinical practice. Therefore, further research on more clinical patients is necessary. Moreover, the sample size of our study was small, and our conclusions might not be clinically convincing enough. In short, our new device needs further clinical research.
Conclusions
The new device we have developed creatively adopts the shoulder-hip compression and pneumatic pressure modes. In our study of asymptomatic volunteers, all individuals completed their examinations successfully, with satisfactory image quality and no significant discomfort caused by the new device. The DSCA, SVCD, and DH at three disc levels changed to a certain extent, with the DSCA and SVCD at L4-5 decreasing significantly. Future studies with clinical patients should be designed to confirm whether the new device can improve the accuracy of diagnosis of lumbar degenerative diseases.
Acknowledgments
Funding: This work was supported the General Program of the Special Project of Military Health Care (No. 18BJZ43).
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://qims.amegroups.com/article/view/10.21037/qims-22-283/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the Institutional Review Board of the 305 Hospital of PLA, Beijing, and informed consent was obtained from all the participants.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Vroomen PC, de Krom MC, Wilmink JT, Kester AD, Knottnerus JA. Diagnostic value of history and physical examination in patients suspected of lumbosacral nerve root compression. J Neurol Neurosurg Psychiatry 2002;72:630-4. [Crossref] [PubMed]
- Rainville J, Lopez E. Comparison of radicular symptoms caused by lumbar disc herniation and lumbar spinal stenosis in the elderly. Spine (Phila Pa 1976) 2013;38:1282-7. [Crossref] [PubMed]
- Kreiner DS, Hwang SW, Easa JE, Resnick DK, Baisden JL, Bess S, et al. An evidence-based clinical guideline for the diagnosis and treatment of lumbar disc herniation with radiculopathy. Spine J 2014;14:180-91. [Crossref] [PubMed]
- de Graaf I, Prak A, Bierma-Zeinstra S, Thomas S, Peul W, Koes B. Diagnosis of lumbar spinal stenosis: a systematic review of the accuracy of diagnostic tests. Spine (Phila Pa 1976) 2006;31:1168-76. [Crossref] [PubMed]
- Karadimas EJ, Siddiqui M, Smith FW, Wardlaw D. Positional MRI changes in supine versus sitting postures in patients with degenerative lumbar spine. J Spinal Disord Tech 2006;19:495-500. [Crossref] [PubMed]
- Oren O, Kebebew E, Ioannidis JPA. Curbing Unnecessary and Wasted Diagnostic Imaging. JAMA 2019;321:245-6. [Crossref] [PubMed]
- Brinjikji W, Luetmer PH, Comstock B, Bresnahan BW, Chen LE, Deyo RA, Halabi S, Turner JA, Avins AL, James K, Wald JT, Kallmes DF, Jarvik JG. Systematic literature review of imaging features of spinal degeneration in asymptomatic populations. AJNR Am J Neuroradiol 2015;36:811-6. [Crossref] [PubMed]
- Hebelka H, Rydberg N, Hutchins J, Lagerstrand K, Brisby H. Axial Loading during MRI Induces Lumbar Foraminal Area Changes and Has the Potential to Improve Diagnostics of Nerve Root Compromise. J Clin Med 2022;11:2122. [Crossref] [PubMed]
- Sasani H, Solmaz B, Sasani M, Vural M, Ozer AF. Diagnostic Importance of Axial Loaded Magnetic Resonance Imaging in Patients with Suspected Lumbar Spinal Canal Stenosis. World Neurosurg 2019;127:e69-75. [Crossref] [PubMed]
- Kim YK, Lee JW, Kim HJ, Yeom JS, Kang HS. Diagnostic advancement of axial loaded lumbar spine MRI in patients with clinically suspected central spinal canal stenosis. Spine (Phila Pa 1976) 2013;38:E1342-7. [Crossref] [PubMed]
- Kinder A, Filho FP, Ribeiro E, Domingues RC, Domingues RC, Marchiori E, Gasparetto E. Magnetic resonance imaging of the lumbar spine with axial loading: a review of 120 cases. Eur J Radiol 2012;81:e561-4. [Crossref] [PubMed]
- Willén J, Danielson B. The diagnostic effect from axial loading of the lumbar spine during computed tomography and magnetic resonance imaging in patients with degenerative disorders. Spine (Phila Pa 1976) 2001;26:2607-14. [Crossref] [PubMed]
- Fiani B, Griepp DW, Lee J, Davati C, Moawad CM, Kondilis A. Weight-Bearing Magnetic Resonance Imaging as a Diagnostic Tool That Generates Biomechanical Changes in Spine Anatomy. Cureus 2020;12:e12070. [Crossref] [PubMed]
- Nordberg CL, Hansen BB, Nybing JD, Hansen P, Bliddal H, Griffith JF, Fournier G, Guglielmi G, Boesen M. Weight-bearing MRI of the Lumbar Spine: Technical Aspects. Semin Musculoskelet Radiol 2019;23:609-20. [Crossref] [PubMed]
- Sato K, Kikuchi S, Yonezawa T. In vivo intradiscal pressure measurement in healthy individuals and in patients with ongoing back problems. Spine (Phila Pa 1976) 1999;24:2468-74. [Crossref] [PubMed]
- Hebelka H, Torén L, Lagerstrand K, Brisby H. Axial loading during MRI reveals deviant characteristics within posterior IVD regions between low back pain patients and controls. Eur Spine J 2018;27:2840-6. [Crossref] [PubMed]
- Schober P, Mascha EJ, Vetter TR. Statistics From A (Agreement) to Z (z Score): A Guide to Interpreting Common Measures of Association, Agreement, Diagnostic Accuracy, Effect Size, Heterogeneity, and Reliability in Medical Research. Anesth Analg 2021;133:1633-41. [Crossref] [PubMed]
- Nilsson M, Lagerstrand K, Kasperska I, Brisby H, Hebelka H. Axial loading during MRI influences T2-mapping values of lumbar discs: a feasibility study on patients with low back pain. Eur Spine J 2016;25:2856-63. [Crossref] [PubMed]
- Torén L, Hebelka H, Kasperska I, Brisby H, Lagerstrand K. With axial loading during MRI diurnal T2-value changes in lumbar discs are neglectable: a cross sectional study. BMC Musculoskelet Disord 2018;19:25. [Crossref] [PubMed]
- Hioki A, Miyamoto K, Shimizu K, Inoue N. Test-retest repeatability of lumbar sagittal alignment and disc height measurements with or without axial loading: a computed tomography study. J Spinal Disord Tech 2011;24:93-8. [Crossref] [PubMed]
- Hjaltadottir H, Hebelka H, Molinder C, Brisby H, Baranto A. Axial loading during MRI reveals insufficient effect of percutaneous interspinous implants (Aperius™ PerCLID™) on spinal canal area. Eur Spine J 2020;29:122-8. [Crossref] [PubMed]
- Willén J, Danielson B, Gaulitz A, Niklason T, Schönström N, Hansson T. Dynamic effects on the lumbar spinal canal: axially loaded CT-myelography and MRI in patients with sciatica and/or neurogenic claudication. Spine (Phila Pa 1976) 1997;22:2968-76. [Crossref] [PubMed]
- Ozawa H, Kanno H, Koizumi Y, Morozumi N, Aizawa T, Kusakabe T, Ishii Y, Itoi E. Dynamic changes in the dural sac cross-sectional area on axial loaded MR imaging: is there a difference between degenerative spondylolisthesis and spinal stenosis? AJNR Am J Neuroradiol 2012;33:1191-7. [Crossref] [PubMed]
- Kimura S, Steinbach GC, Watenpaugh DE, Hargens AR. Lumbar spine disc height and curvature responses to an axial load generated by a compression device compatible with magnetic resonance imaging. Spine (Phila Pa 1976) 2001;26:2596-600. [Crossref] [PubMed]
- Hioki A, Miyamoto K, Sakai H, Shimizu K. Lumbar axial loading device alters lumbar sagittal alignment differently from upright standing position: a computed tomography study. Spine (Phila Pa 1976) 2010;35:995-1001. [Crossref] [PubMed]
- Kanno H, Aizawa T, Ozawa H, Koizumi Y, Morozumi N, Itoi E. An increase in the degree of olisthesis during axial loading reduces the dural sac size and worsens clinical symptoms in patients with degenerative spondylolisthesis. Spine J 2018;18:726-33. [Crossref] [PubMed]
- Danielson B, Willén J. Axially loaded magnetic resonance image of the lumbar spine in asymptomatic individuals. Spine (Phila Pa 1976) 2001;26:2601-6. [Crossref] [PubMed]
- Marques JP, Simonis FFJ, Webb AG. Low-field MRI: An MR physics perspective. J Magn Reson Imaging 2019;49:1528-42. [Crossref] [PubMed]
- Charest-Morin R, Zhang H, Shewchuk JR, Wilson DR, Phillips AE, Bond M, Street J. Dynamic morphometric changes in degenerative lumbar spondylolisthesis: A pilot study of upright magnetic resonance imaging. J Clin Neurosci 2021;91:152-8. [Crossref] [PubMed]
- Berry DB, Hernandez A, Onodera K, Ingram N, Ward SR, Gombatto SP. Lumbar spine angles and intervertebral disc characteristics with end-range positions in three planes of motion in healthy people using upright MRI. J Biomech 2019;89:95-104. [Crossref] [PubMed]
- Botchu R, Bharath A, Davies AM, Butt S, James SL. Current concept in upright spinal MRI. Eur Spine J 2018;27:987-93. [Crossref] [PubMed]
- Splendiani A, Perri M, Grattacaso G, Di Tunno V, Marsecano C, Panebianco L, Gennarelli A, Felli V, Varrassi M, Barile A, Di Cesare E, Masciocchi C, Gallucci M. Magnetic resonance imaging (MRI) of the lumbar spine with dedicated G-scan machine in the upright position: a retrospective study and our experience in 10 years with 4305 patients. Radiol Med 2016;121:38-44. [Crossref] [PubMed]
- Zeifang F, Schiltenwolf M, Abel R, Moradi B. Gait analysis does not correlate with clinical and MR imaging parameters in patients with symptomatic lumbar spinal stenosis. BMC Musculoskelet Disord 2008;9:89. [Crossref] [PubMed]
- Madsen R, Jensen TS, Pope M, Sørensen JS, Bendix T. The effect of body position and axial load on spinal canal morphology: an MRI study of central spinal stenosis. Spine (Phila Pa 1976) 2008;33:61-7. [Crossref] [PubMed]
- Kanno H, Endo T, Ozawa H, Koizumi Y, Morozumi N, Itoi E, Ishii Y. Axial loading during magnetic resonance imaging in patients with lumbar spinal canal stenosis: does it reproduce the positional change of the dural sac detected by upright myelography? Spine (Phila Pa 1976) 2012;37:E985-92. [Crossref] [PubMed]
- Hiwatashi A, Danielson B, Moritani T, Bakos RS, Rodenhause TG, Pilcher WH, Westesson PL. Axial loading during MR imaging can influence treatment decision for symptomatic spinal stenosis. AJNR Am J Neuroradiol 2004;25:170-4. [PubMed]
- Mahato NK, Sybert D, Law T, Clark B. Effects of spine loading in a patient with post-decompression lumbar disc herniation: observations using an open weight-bearing MRI. Eur Spine J 2017;26:17-23. [Crossref] [PubMed]


