
Measuring glenoid and humeral bone loss in shoulder dislocation
Background
Glenoid bone loss (GBL) is common following shoulder dislocation, being apparent in about 40% of patients with a single dislocation and 85% of patients with recurrent dislocation (1). It results from impaction of the humeral head against the anterior glenoid rim at the time of dislocation. GBL occurs along the anterior aspect of the glenoid (2), though as the glenoid has an anteroinferior orientation, this bone loss may appear to be present antero-inferiorly rather than anteriorly (3).
Most (80%) GBL occurs from a compression fracture rather than a fragmented fracture (1). Only modest correlation (r=0.56) exists between the number of dislocations and the severity of the GBL (1); rather, the force of dislocation may be more relevant. For instance, a single violent anterior dislocation following, for example, a road traffic accident, may produce as much GBL as several episodes of less violent anterior dislocation.
The middle one-third of the glenoid is composed of very thick bone while the glenoid bone gradually thins as one moves peripherally. The normal anterior glenoid rim is curved. As bone is lost, the anterior glenoid rim becomes progressively straighter and the glenoid width becomes progressively narrower. With more severe degrees of GBL, as the thicker middle one-third of the glenoid is approached, bone loss becomes concentrated in the middle one-third of the anterior glenoid leading to an anterior concavity (2).
GBL reduces the contact area between the humeral head and the glenoid. As a result, dislocation can occur more easily in a downward spiral with easier dislocation leading to more GBL leading to more dislocations and so forth (Figure 1). Severe GBL increasingly facilitates relocation such that some patients may experience up to 2,000 anterior dislocations, dislocating and relocating with considerable ease.

Quantifying glenoid bone loss (GBL)
GBL can be quantified using radiographs, computed tomography (CT), or magnetic resonance imaging (MRI). Radiographs seem to be quite accurate but can require a high level of radiographic expertise to acquire the correct projection. Radiographs are also limited in that they cannot reliably measure glenoid track.
The preferred method for the most accurate assessment of GBL is CT with comparison of the affected side to the contralateral unaffected side. Information regarding the contralateral side is always available when one shoulder is examined by CT so it makes sense to use this readily available CT data. There is no increase in patient dose. One does need to ensure that the radiographer reconstructs the image data for both shoulders rather than just one shoulder (Figure 2). As there is almost perfect symmetry between the shape and the size of both glenoid fossae (4), the contralateral glenoid can be reliably used as a reference to initial glenoid size provided there is no evidence of GBL on the contralateral side from bilateral dislocation. Using the contralateral glenoid to measure GBL is more accurate than measuring GBL on the affected side alone (4,5).
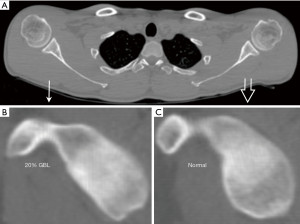
Because of the slanting orientation of the glenoid, it is difficult to judge GBL on axial images alone, and reconstructed images en face to the glenoid surface should be obtained (Figure 2). More practically, 2D reconstructed double oblique views en face to the glenoid rather than 3D views are accurate and easier to obtain (5). 3D reconstructions provide a better perception of GBL though are more time-consuming to obtain and may be less accurate with respect to actual measurements as the margins are not as sharply delineated. One could ideally undertake measurements using double oblique views en face to the glenoid and also then obtain 3D reconstructions for perceptional representation. A teaching video on how to easily obtain double oblique views of the glenoid on the standard workstation together with a standard radiological report for GBL can be viewed at http://www.droid.cuhk.edu.hk/special.htm.
With MRI, only a single shoulder is usually available, and, in this instance, the best fit circle method is the preferred technique for MRI assessment. While not as accurate as a comparison with the contralateral shoulder, the best fit circle method is still reasonably accurate and provides a good estimate as to the severity of GBL. However, the best fit circle method can overestimate GBL by at least 5% due to differences in the contour between the anterior and posterior margins of the glenoid (6). This overestimation is greatest when there is moderate to severe bone loss (6). Nevertheless, in many instances, MR assessment of glenoid and humeral bone loss alone suffices. When more accurate measurements are required, as in determination of glenoid track, CT is probably the preferred technique.
What constitutes a critical level of GBL? This can be considered from two standpoints. First, it can be considered to be that critical level where the frequency of dislocation tends to increase. This has been estimated to be about 13% (1). Second, it can be considered to be at a critical level when capsular repair alone will not suffice to prevent further dislocation. This has been estimated to be about 25% (7). The maximum GBL incurred is about 33% (1). This stands to reason, since, at this measure, bone loss has progressed enough to encounter the thick middle one-third of the scapula, beyond which further bone loss is unlikely.
Measurement of GBL
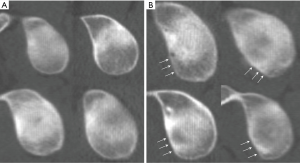
The anterior straight-line
The normal anterior glenoid rim has a smooth curved configuration. An anterior straight-line is the earliest sign of GBL (1,2) (Figure 3). If there is no anterior straight-line on the CT or MR en face view of the glenoid, then there is no GBL present and there is no need to measure GBL. As GBL progresses, the anterior straight-line lengthens. With severe degrees of GBL, the anterior curvature of the glenoid becomes concave (2) (Figure 4). Any time one sees an anterior concavity to the glenoid, one can immediately infer severe GBL (2).
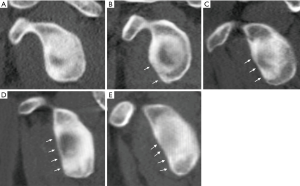
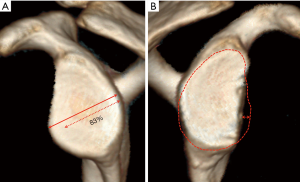
Measuring GBL on CT using the contralateral shoulder
Once a good quality en face view of the glenoid has been obtained, two lines are drawn on this image. The first is a line along the long axis of the glenoid from the supraglenoid tubercle region to the most inferior part of the glenoid. This is a reference line. The second line is drawn at right angles to this long axis at the inferior half of the glenoid, measuring the maximum width of the glenoid surface. This is the key measurement line. Its accuracy is dependent on obtaining the best possible en face view to the glenoid with clear demarcation of the anterior and posterior margins of the inferior part of the glenoid.
The same reconstruction is performed, and lines drawn on the contralateral unaffected shoulder, which is used as an internal guide to the original size and configuration of the glenoid. The degree of GBL can thus be accurately determined (Figure 5).

Measurement of GBL on MRI using best fit circle method
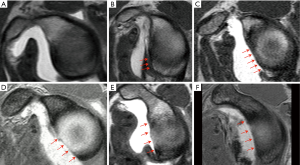
Most shoulder dislocations are evaluated with MRI and not CT. It makes sense to evaluate the degree of GBL on MRI (8) (Figure 6). In many instances doing so negates the need for additional CT examination. Overall CT with comparison of the contralateral side is slightly more accurate than MRI examination, although MRI should suffice for most clinical indications (8).
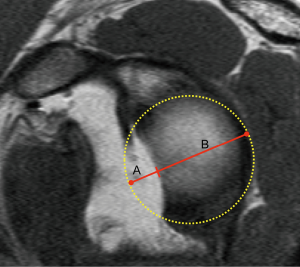
MRI accuracy depends on obtaining a good quality dedicated en face view of the glenoid surface. This high-resolution image en face through the glenoid surface should be planned from axial, coronal and sagittal images (8). Relying on standard sagittal images may not always provide a good en face view through the glenoid.
Once a high quality en face view has been obtained, one should first look for an anterior straight-line. If there is no anterior straight-line to the anterior glenoid rim, there is no GBL present and no need for further measurements. If an anterior straight-line is present, then one needs to proceed with GBL measurements (Figure 7). As the contralateral shoulder is not available for comparison, a best fit circle method is used. This circle should be planned to fit as close as possible the posterior and inferior margins of the inferior glenoid (8) (Figure 6). The diameter of the circle approximates to normal glenoid shape (Figure 6).
Hill Sachs deformity
Hill Sachs deformity is present in 81% of patients following single dislocation and 87% of patients with recurrent dislocation (1). Occasionally Hill Sachs deformity may be present in the absence of any GBL and vice versa. All patients with recurrent dislocation have either GBL or Hill Sachs deformity such that absence of these deformities makes the likelihood of recurrent anterior shoulder dislocation extremely unlikely (1).
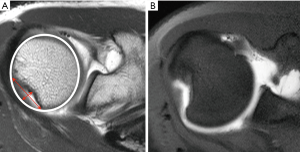
A Hill Sachs deformity is located at the posterior aspect of the humeral head extending from 0–24 mm from the proximal end of the humeral head (9). Usually, a small Hill Sachs deformity is located close to the greater tuberosity with larger lesions extending more medially towards the articular surface of the proximal humerus (10). One should note whether the Hill Sachs deformity is flattened or angulated as the latter, which is less common, may have a greater propensity to engage with the anterior glenoid rim (Figure 8).
A Hill-Sachs deformity is not related to mid-range stability because, in this situation, it is positioned away from the edge of the glenoid. A Hill Sachs deformity only comes into play at the end range of stability such as abduction and external rotation, where it can engage with the anterior rim of the glenoid (3).
Measurement of Hill Sachs deformity
Hill Sachs deformity should be assessed on orthogonal planes though it is best measured on axial images at the more superior aspect of the proximal humerus above the level of the coracoid process (11). The widest width of the Hill Sachs deformity, which is the most important measure, with regard to glenoid track (see below) can be measured from axial CT or MRI measurements (Figure 8). A best fit circle through the superior aspect of the proximal humerus can be used to determine the depth of a Hill Sachs deformity.
Glenoid track
The glenoid track is a concept that addresses the interaction between the glenoid and the humeral head during shoulder movement (12,13). It defines the contact area between these two bone areas during maximum external rotation, maximum extension and 90° abduction. The glenoid track was measured initially on cadavers (14) and later on patients using an open MR system and 3D motion analysis software (15). The mean width of the glenoid track at 90° arm abduction was shown to be 83% of the full glenoid width. In other words, the humeral head utilizes 83% of the glenoid width between neutral and 90° arm abduction. Therefore, it was recommended that one should use 83% of the normal glenoid width as the glenoid track width (15).
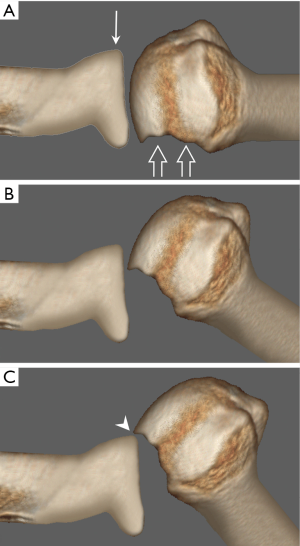
Following shoulder dislocation, glenoid track is measured to determine the likelihood of the Hill Sachs deformity passing beyond, and thereby engaging with, the anterior rim of the glenoid during abduction and external rotation (14) (Figures 9,10). This measure enables the surgeon to preoperatively predict the likelihood of failure following Bankart repair (16). Surgeons do not like to test this stability immediately after surgery as it may increase the risk of failure (17). In such instances where the Hill-Sachs deformity is likely to pass beyond the anterior glenoid rim, during abduction and external rotation, the surgeon may consider more extensive surgery with augmentation of either the GBL ± the Hill Sachs deformity (16). Measurements of glenoid track can be undertaken on reconstructed 2D CT (18), 3D CT (13) or MRI images (11). The glenoid track concept does not apply to the small percentage of patients without a Hill Sachs deformity (16). With bipolar (i.e., both glenoid and humeral bone loss), two elements need to be measured, namely glenoid track and humeral interval.
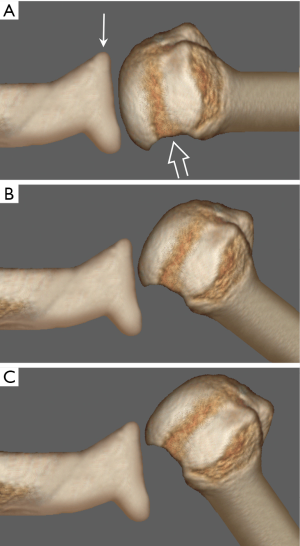
Glenoid track (mm) =83% of normal glenoid width (mm) − GBL (mm) (Figure 11).
Humeral interval (mm) = maximum width of Hill Sachs defect (mm) + bony bridge between Hill Sachs lesion and medial border of the rotator cuff attachment (Figure 12).
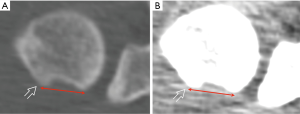
The humeral interval is the width of the Hill Sachs deformity together with the adjacent bone bridge between the Hill Sachs deformity and the rotator cuff tendon insertion (17,19). The insertion of the rotator cuff tendons, which in this case refers to the teres minor and infraspinatus tendons, is difficult to define on CT images, even on a soft-tissue window setting, so one has to estimate this insertion.
On-track and off-track lesions
If the glenoid track is less than the width of the humeral interval, the lesion is defined as being off-track (16,17). This means that, in such cases, the edge of the Hill Sachs lesion is likely to extend beyond the anterior margin of the anterior glenoid during maximum abduction. Generally, about 15–20% of lesions tend to be off track (11,16). Glenoid track estimation of on-track or off-track lesions has moderate to high accuracy in predicting the likelihood of engagement at surgery (11), in addition to the likelihood of recurrence following arthroscopic Bankart reconstruction (20).
Variability of glenoid track measurements
There is a high level of agreement (>90%) between and within observers for linear GBL measurements (21). Moderate to good interobserver (~65%) and good interobserver agreement (~85%) exists for determining on-track or off-track lesions (21). Most variation results from determining the site of insertion and margins of the Hill Sachs lesion. These features seem to be more readily appreciated on two-dimensional rather than three-dimensional images and are more readily apparent on MRI than CT.
Acknowledgements
None.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- Griffith JF, Antonio GE, Yung PS, Wong EM, Yu AB, Ahuja AT, Chan KM. Prevalence, pattern, and spectrum of glenoid bone loss in anterior shoulder dislocation: CT analysis of 218 patients. AJR Am J Roentgenol 2008;190:1247-54. [Crossref] [PubMed]
- Griffith JF, Antonio GE, Tong CW, Ming CK. Anterior shoulder dislocation: quantification of glenoid bone loss with CT. AJR Am J Roentgenol 2003;180:1423-30. [Crossref] [PubMed]
- Itoi E. 'On-track' and 'off-track' shoulder lesions. EFORT Open Rev 2017;2:343-51. [Crossref] [PubMed]
- Shi L, Griffith JF, Huang J, Wang D. Excellent side-to-side symmetry in glenoid size and shape. Skeletal Radiol 2013;42:1711-5. [Crossref] [PubMed]
- Griffith JF, Yung PS, Antonio GE, Tsang PH, Ahuja AT, Chan KM. CT compared with arthroscopy in quantifying glenoid bone loss. AJR Am J Roentgenol 2007;189:1490-3. [Crossref] [PubMed]
- Lansdown DA, Wang K, Bernardoni E, Frank RM, Yanke AB, Cole BJ, Verma NN, Romeo AA. Variability in the Contour of Cadaveric Anterior and Posterior Glenoids Based on Ipsilateral 3-Dimensional Computed Tomography Reconstructions: Implications for Clinical Estimation of Bone Loss. Arthroscopy 2018;34:2560-6. [Crossref] [PubMed]
- Yamamoto N, Itoi E, Abe H, Kiluchi K, Seki N, Minagawa H, Tuoheti Y. Effect of an anterior glenoid defect on anterior shoulder stability: a cadaveric study. Am J Sports Med 2009;37:949-54. [Crossref] [PubMed]
- Lee RK, Griffith JF, Tong MM, Sharma N, Yung P. Glenoid bone loss: assessment with MR imaging. Radiology 2013;267:496-502. [Crossref] [PubMed]
- Saito H, Itoi E, Minagawa H, Yamamoto N, Tuoheti Y, Seki N. Location of the Hill-Sachs lesion in shoulders with recurrent anterior dislocation. Arch Orthop Trauma Surg 2009;129:1327-34. [Crossref] [PubMed]
- Kurokawa D, Yamamoto N, Nagamoto H, Omori Y, Tanaka M, Sano H, Itoi E. The prevalence of a large Hill Sachs lesion that needs to be treated. J Shoulder Elbow Surg 2013;22:1285-9. [Crossref] [PubMed]
- Gyftopoulos S, Beltran LS, Bookman J, Rokito A. MRI Evaluation of Bipolar Bone Loss Using the On-Track Off-Track Method: A Feasibility Study. AJR Am J Roentgenol 2015;205:848-52. [Crossref] [PubMed]
- Di Giacomo G, Itoi E, Burkhart SS. Evolving concept of bipolar bone loss and the Hill-Sachs lesion: From ‘engaging/non-engaging’ lesion to ‘on-track/off-track’ lesion. Arthroscopy 2014;30:90-8. [Crossref] [PubMed]
- Momaya AM, Tokish JM. Applying the Glenoid Track Concept in the Management of Patients with Anterior Shoulder Instability. Curr Rev Musculoskelet Med 2017;10:463-8. [Crossref] [PubMed]
- Yamamoto N, Itoi E, Abe H, Minagawa H, Seki N, Shimada Y, Okada K. Contact between the glenoid and the humeral head in abduction, external rotation, and horizontal extension: a new concept of glenoid track. J Shoulder Elbow Surg 2007;16:649-56. [Crossref] [PubMed]
- Omori Y, Yamamoto N, Koishi H, Futai K, Goto A, Sugamoto K, Itoi E. Measurement of the glenoid track in vivo as investigated by 3-dimensional motion analysis using open MRI. Am J Sports Med 2014;42:1290-5. [Crossref] [PubMed]
- Shaha JS, Cook JB, Rowles DJ, Bottoni CR, Shaha SH, Tokish JM. Clinical Validation of the Glenoid Track Concept in Anterior Glenohumeral Instability. J Bone Joint Surg Am 2016;98:1918-23. [Crossref] [PubMed]
- Younan Y, Wong PK, Karas S, Umpierrez M, Gonzalez F, Jose J, Singer AD. The glenoid track: a review of the clinical relevance, method of calculation and current evidence behind this method. Skeletal Radiol 2017;46:1625-34. [Crossref] [PubMed]
- Burns DM, Chahal J, Shahrokhi S, Henry P, Wasserstein D, Whyne C, Theodoropoulos J, Ogilvie-Harris D, Dwyer T. Diagnosis of Engaging Bipolar Bone Defects in the Shoulder Using 2-Dimensional Computed Tomography: A Cadaveric Study. Am J Sports Med 2016;44:2771-7. [Crossref] [PubMed]
- Gulati A, Dessouky R, Wadhwa V, Sanders D, Chhabra A. New concepts of radiologic preoperative evaluation of anterior shoulder instability: on-track and off-track lesions. Acta Radiol 2018;59:966-72. [Crossref] [PubMed]
- Locher J, Wilken F, Beitzel K, Buchmann S, Longo UG, Denaro V, Imhoff AB. Hill-Sachs Off-track lesions as risk factor for recurrence of instability after arthroscopic Bankart repair. Arthroscopy 2016;32:1993-9. [Crossref] [PubMed]
- Schneider AK, Hoy GA, Ek ET, Rotstein AH, Tate J, Taylor DM, Evans MC. Interobserver and intraobserver variability of glenoid track measurements. J Shoulder Elbow Surg 2017;26:573-9. [Crossref] [PubMed]


